- Record: found
- Abstract: found
- Article: found
Brain network disintegration as a final common pathway for delirium: a systematic review and qualitative meta-analysis
Read this article at
Abstract
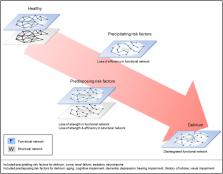
Delirium is an acute neuropsychiatric syndrome characterized by altered levels of attention and awareness with cognitive deficits. It is most prevalent in elderly hospitalized patients and related to poor outcomes. Predisposing risk factors, such as older age, determine the baseline vulnerability for delirium, while precipitating factors, such as use of sedatives, trigger the syndrome. Risk factors are heterogeneous and the underlying biological mechanisms leading to vulnerability for delirium are poorly understood. We tested the hypothesis that delirium and its risk factors are associated with consistent brain network changes. We performed a systematic review and qualitative meta-analysis and included 126 brain network publications on delirium and its risk factors. Findings were evaluated after an assessment of methodological quality, providing N=99 studies of good or excellent quality on predisposing risk factors, N=10 on precipitation risk factors and N=7 on delirium. Delirium was consistently associated with functional network disruptions, including lower EEG connectivity strength and decreased fMRI network integration. Risk factors for delirium were associated with lower structural connectivity strength and less efficient structural network organization. Decreased connectivity strength and efficiency appear to characterize structural brain networks of patients at risk for delirium, possibly impairing the functional network, while functional network disintegration seems to be a final common pathway for the syndrome.
Highlights
-
•
Delirium is consistently associated with functional network impairments.
-
•
Risk factors are associated with lower structural connectivity strength.
-
•
Risk factors are associated with a less efficient structural network organization.
-
•
Structural impairments make the functional network more vulnerable to deterioration.
-
•
Functional network disintegration seems to be a final common pathway for delirium.
Related collections
Most cited references129
- Record: found
- Abstract: found
- Article: not found
Benchmarking of participant-level confound regression strategies for the control of motion artifact in studies of functional connectivity.
- Record: found
- Abstract: found
- Article: not found
Structural insights into aberrant topological patterns of large-scale cortical networks in Alzheimer's disease.
- Record: found
- Abstract: found
- Article: not found