- Record: found
- Abstract: found
- Article: found
Beta-blockers in cirrhosis: Evidence-based indications and limitations
Read this article at
Summary
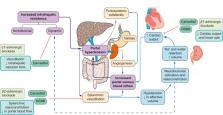
Non-selective beta-blockers (NSBBs) are the mainstay of treatment for portal hypertension in the setting of liver cirrhosis. Randomised controlled trials demonstrated their efficacy in preventing initial variceal bleeding and subsequent rebleeding. Recent evidence indicates that NSBBs could prevent liver decompensation in patients with compensated cirrhosis. Despite solid data favouring NSBB use in cirrhosis, some studies have highlighted relevant safety issues in patients with end-stage liver disease, particularly with refractory ascites and infection. This review summarises the evidence supporting current recommendations and restrictions of NSBB use in patients with cirrhosis.
Related collections
Most cited references73
- Record: found
- Abstract: found
- Article: not found
Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients.
- Record: found
- Abstract: found
- Article: not found