- Record: found
- Abstract: found
- Article: found
Improving CT-guided transthoracic biopsy of mediastinal lesions by diffusion-weighted magnetic resonance imaging
Read this article at
Abstract
OBJECTIVES:
To evaluate the preliminary results obtained using diffusion-weighted magnetic resonance imaging and the apparent diffusion coefficient for planning computed tomography-guided biopsies of selected mediastinal lesions.
METHODS:
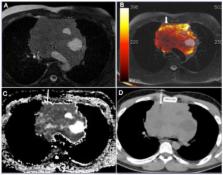
Eight patients with mediastinal lesions suspicious for malignancy were referred for computed tomography-guided biopsy. Diffusion-weighted magnetic resonance imaging and apparent diffusion coefficient measurement were performed to assist in biopsy planning with diffusion/computed tomography fused images. We selected mediastinal lesions that could provide discordant diagnoses depending on the biopsy site, including large heterogeneous masses, lesions associated with lung atelectasis or consolidation, lesions involving large mediastinal vessels and lesions for which the results of biopsy using other methods and histopathological examination were divergent from the clinical and radiological suspicion.
RESULTS:
In all cases, the biopsy needle was successfully directed to areas of higher signal intensity on diffusion-weighted sequences and the lowest apparent diffusion coefficient within the lesion (mean, 0.8 [range, 0.6–1.1]×10 -3 mm 2/s), suggesting high cellularity. All biopsies provided adequate material for specific histopathological diagnoses of four lymphomas, two sarcomas and two thymomas.
CONCLUSION:
Functional imaging tools, such as diffusion-weighted imaging and the apparent diffusion coefficient, are promising for implementation in noninvasive and imaging-guided procedures. However, additional studies are needed to confirm that mediastinal biopsy can be improved with these techniques.
Related collections
Most cited references72
- Record: found
- Abstract: found
- Article: not found
Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations.
- Record: found
- Abstract: found
- Article: not found