- Record: found
- Abstract: found
- Article: found
Echocardiographic Predictors of Worse Outcome After Cardiac Resynchronization Therapy
Read this article at
Abstract
Background
Cardiac resynchronization therapy (CRT) is the recommended treatment by leading global guidelines. However, 30%-40% of selected patients are non-responders.
Objective
To develop an echocardiographic model to predict cardiac death or transplantation (Tx) 1 year after CRT.
Method
Observational, prospective study, with the inclusion of 116 patients, aged 64.89 ± 11.18 years, 69.8% male, 68,1% in NYHA FC III and 31,9% in FC IV, 71.55% with left bundle-branch block, and median ejection fraction (EF) of 29%. Evaluations were made in the pre-implantation period and 6-12 months after that, and correlated with cardiac mortality/Tx at the end of follow-up. Cox and logistic regression analyses were performed with ROC and Kaplan-Meier curves. The model was internally validated by bootstrapping.
Results
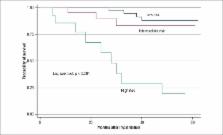
There were 29 (25%) deaths/Tx during follow-up of 34.09 ± 17.9 months. Cardiac mortality/Tx was 16.3%. In the multivariate Cox model, EF < 30%, grade III/IV diastolic dysfunction and grade III mitral regurgitation at 6-12 months were independently related to increased cardiac mortality or Tx, with hazard ratios of 3.1, 4.63 and 7.11, respectively. The area under the ROC curve was 0.78.
Related collections
Most cited references27
- Record: found
- Abstract: not found
- Article: not found
American Society of Echocardiography recommendations for use of echocardiography in clinical trials.
- Record: found
- Abstract: found
- Article: not found
Left ventricular reverse remodeling but not clinical improvement predicts long-term survival after cardiac resynchronization therapy.
- Record: found
- Abstract: found
- Article: not found