- Record: found
- Abstract: found
- Article: found
The clinical–epidemiological profile of malaria patients from Southern Venezuela, a critical hotspot in Latin America
Read this article at
Abstract
Background
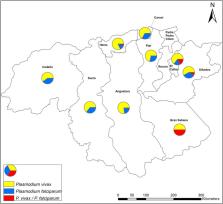
Venezuela accounted for 55% of the cases and 73% of the malaria deaths in the Americas in 2019. Bolivar state, in the southeast, contributes > 60% of the country's Plasmodium vivax and Plasmodium falciparum cases every year. This study describes the clinical–epidemiological characteristics of clinical malaria patients in this high-transmission area.
Methods
A prospective study was conducted on patients seeking medical attention in three medical centres in the state capital, Ciudad Bolivar, between June and October 2018. Malaria diagnosis was carried out using microscopy following national standards. Malaria-positive patients were examined for clinical symptoms, and haematological tests were performed at the time of diagnosis. Patients were followed up by telephone to evaluate malaria recurrences.
Results
Out of 287 patients, 200 (69.7%) were positive for P. vivax, 69 (24%) for P. falciparum, and 18 (6.3%) had mixed ( P. vivax/ P. falciparum) infections. Patients' median age was 33 years (IQR 20), 168 (69%) were men, and 40% practiced gold mining as the main occupation. Fever (96.5%), chills (91.3%), and headaches (90.6%) were the most frequent symptoms. At least one symptom associated with severe malaria was observed in 69 out of 161 patients with complete clinical evaluation (42.9%). Plasmodium vivax infections were found in 42 out of 69 (60.9%) severe cases; by contrast, P. falciparum and mixed malaria caused 34.8% (24/69) and 4.4% (3/69) of infections, respectively. Two patients died of cerebral malaria. Mean hemoglobin was lower in the patients infected with P. falciparum than those infected with P. vivax. Regardless of the parasite causing the infection, patients presented high levels of total bilirubin, aminotransferases (AST, ALT), and lactate dehydrogenase (LDH). Out of the 142 patients followed up by phone for three months (49.5% of the 287 patients), 35 (24.7%) reported recurrences.
Conclusions
The high malaria prevalence among young male adults practicing gold mining suggests that this occupation is a significant risk factor. The unexpected high prevalence of P. vivax patients with at least one criteria of severe clinical disease is a matter of concern. Whether it is the result of a lack of timely diagnosis and effective treatment should be explored.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Geographical variation in Plasmodium vivax relapse
- Record: found
- Abstract: found
- Article: not found