- Record: found
- Abstract: found
- Article: found
What is the most cost‐effective strategy for nasal screening and Staphylococcus aureus decolonization in patients undergoing total hip arthroplasty?
Read this article at
Abstract
Background
To reduce periprosthetic joint infection after total hip arthroplasty (THA), several nasal screening and decolonization strategies for methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive Staphylococcus aureus (MSSA) have been performed. These include universal decolonization (UD; i.e., no screening and decolonization for all patients), universal screening and target decolonization (US; i.e., screening for all patients and decolonization for bacterial positive patients), and target screening and decolonization (TS; i.e., screening and decolonization for high-risk populations only). Although TS is the most cost-effective strategy, useful risk factors must be identified. The purpose of this study was to evaluate the presence of predictive factors that enable the TS strategy to be successfully implemented and to compare the costs of each strategy.
Methods
A total of 1654 patients scheduled for primary or revision THA (1464 female, 190 male; mean age 64 years) were screened prior to surgery for bacterial colonization of the nasal mucosa. Risk factors for positive MRSA and S. aureus (including both MRSA and MSSA) tests were analyzed according to the following parameters: sex, age ≥ 80 years, body mass index ≥ 30 kg/m 2, antibiotic use within 3 years, corticosteroid use, serum albumin < 3.5 g/dL, glomerular filtration rate < 50 mL/min, presence of brain, thyroid, cardiac, or pulmonary disease, diabetes, asthma, smoking status, and whether revision surgery was performed. The average cost of each strategy was calculated.
Results
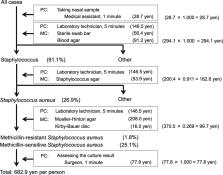
In total, 29 patients (1.8 %) tested positive for MRSA and 445 (26.9 %) tested positive for S. aureus. No parameters were identified as independent risk factors for MRSA and only female sex was identified as a risk factor for S. aureus (p = 0.003; odds ratio: 1.790; 95 % confidence interval: 1.210–2.640). The average cost of each strategy was 1928.3 yen for UD, 717.6 yen for US, and 717.6 yen for TS (for eradicating MRSA), and 1928.3 yen for UD, 1201.6 yen for US, and 1160.4 yen for TS (for eradicating S. aureus).
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
<i>Staphylococcus aureus</i> Infections
- Record: found
- Abstract: found
- Article: not found
Targeted versus universal decolonization to prevent ICU infection.
- Record: found
- Abstract: found
- Article: not found