- Record: found
- Abstract: found
- Article: found
Twenty-Year Change in Severity and Outcome of Ischemic and Hemorrhagic Strokes

Read this article at
Abstract
This cohort study assesses secular changes in initial neurological severity and short-term functional outcomes of patients with acute stroke by sex using a large population.
Key Points
Question
Did the initial neurological severity and functional outcomes of patients with stroke change throughout a 20-year period?
Findings
In this hospital-based, multicenter, prospective registry involving 183 080 patients with acute stroke, initial neurological severity showed a decrease over time in all stroke types. Functional outcome at hospital discharge improved in patients with ischemic stroke but no longer showed improvement after adjustment by reperfusion therapy and others; it did not clearly improve in patients with hemorrhagic stroke.
Abstract
Importance
Whether recent changes in demographic characteristics and therapeutic technologies have altered stroke outcomes remains unknown.
Objective
To determine secular changes in initial neurological severity and short-term functional outcomes of patients with acute stroke by sex using a large population.
Design, Setting, and Participants
This nationwide, hospital-based, multicenter, prospective registry cohort study used the Japan Stroke Data Bank and included patients who developed acute stroke from January 2000 through December 2019. Patients with stroke, including ischemic and hemorrhagic strokes, who registered within 7 days after symptom onset were studied. Modified Rankin Scale scores were assessed at hospital discharge for all patients.
Main Outcomes and Measures
Initial severity was assessed by the National Institutes of Health Stroke Scale for ischemic stroke and intracerebral hemorrhage and by the World Federation of Neurological Surgeons grading for subarachnoid hemorrhage. Outcomes were judged as favorable if the modified Rankin Scale score was 0 to 2 and unfavorable if 5 to 6.
Results
Of 183 080 patients, 135 266 (53 800 women [39.8%]; median [IQR] age, 74 [66-82] years) developed ischemic stroke, 36 014 (15 365 women [42.7%]; median [IQR] age, 70 [59-79] years) developed intracerebral hemorrhage, and 11 800 (7924 women [67.2%]; median [IQR] age, 64 [53-75] years) developed subarachnoid hemorrhage. In all 3 stroke types, median ages at onset increased, and the National Institutes of Health Stroke Scale and World Federation of Neurological Surgeons scores decreased throughout the 20-year period on multivariable analysis. In ischemic stroke, the proportion of favorable outcomes showed an increase over time after age adjustment (odds ratio [OR], 1.020; 95% CI, 1.015-1.024 for women vs OR, 1.015; 95% CI, 1.011-1.018 for men) but then stagnated, or even decreased in men, on multivariate adjustment including reperfusion therapy (OR, 0.997; 95% CI, 0.991-1.003 for women vs OR, 0.990; 95% CI, 0.985-0.994 for men). Unfavorable outcomes and in-hospital deaths decreased in both sexes. In intracerebral hemorrhage, favorable outcomes decreased in both sexes, and unfavorable outcomes and deaths decreased only in women. In subarachnoid hemorrhage, the proportion of favorable outcomes was unchanged, and that of unfavorable outcomes and deaths decreased in both sexes.
Conclusions and Relevance
In this study, functional outcomes improved in patients with ischemic stroke during the past 20 years in both sexes presumably partly owing to the development of acute reperfusion therapy. The outcomes of patients with hemorrhagic stroke did not clearly improve in the same period.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials.
- Record: found
- Abstract: found
- Article: found
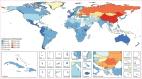
Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016
- Record: found
- Abstract: not found
- Article: not found