- Record: found
- Abstract: found
- Article: found
Development of a triage protocol for patients presenting with gastrointestinal hemorrhage: a prospective cohort study
Read this article at
Abstract
Introduction
Many patients presenting with acute gastrointestinal hemorrhage (GIH) are admitted to the intensive care unit (ICU) for monitoring. A simple triage protocol based upon validated risk factors could decrease ICU utilization.
Methods
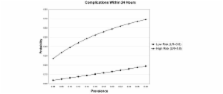
Records of 188 patients admitted with GIH from the emergency department (ED) were reviewed for BLEED criteria (visualized red blood, systolic blood pressure below 100 mm Hg, elevated prothrombin time [PT], erratic mental status, and unstable comorbid disease) and complication within the first 24 hours of admission. Variables associated with early complication were reassessed in 132 patients prospectively enrolled as a validation cohort. A triage model was developed using significant predictors.
Results
We studied 188 patients in the development set and 132 in the validation set. Red blood (relative risk [RR] 4.53, 95% confidence interval [CI] 2.04, 10.07) and elevated PT (RR 3.27, 95% CI 1.53, 7.01) were significantly associated with complication in the development set. In the validation cohort, the combination of red blood or unstable comorbidity had a sensitivity of 0.73, a specificity of 0.55, a positive predictive value of 0.24, and a negative predictive value of 0.91 for complication within 24 hours. In simulation studies, a triage model using these variables could reduce ICU admissions without increasing the number of complications.
Conclusion
Patients presenting to the ED with GIH who have no evidence of ongoing bleeding or unstable comorbidities are at low risk for complication during hospital admission. A triage model based on these variables should be tested prospectively to optimize critical care resource utilization in this common condition.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Risk assessment after acute upper gastrointestinal haemorrhage.
- Record: found
- Abstract: found
- Article: not found
A risk score to predict need for treatment for upper-gastrointestinal haemorrhage.
- Record: found
- Abstract: found
- Article: not found