- Record: found
- Abstract: found
- Article: found
Surgical Assessment of Tissue Quality during Pelvic Organ Prolapse Repair in Postmenopausal Women Pre-Treated Either with Locally Applied Estrogen or Placebo: Results of a Double-Masked, Placebo-Controlled, Multicenter Trial
Read this article at
Abstract
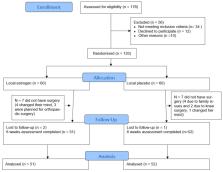
The aim of this prospective randomized, double-masked, placebo-controlled, multicenter study was to analyze the surgeon’s individual assessment of tissue quality during pelvic floor surgery in postmenopausal women pre-treated with local estrogen therapy (LET) or placebo cream. Secondary outcomes included intraoperative and early postoperative course of the two study groups. Surgeons, blinded to patient’s preoperative treatment, completed an 8-item questionnaire after each prolapse surgery to assess tissue quality as well as surgical conditions. Our hypothesis was that there is no significant difference in individual surgical assessment of tissue quality between local estrogen or placebo pre-treatment. Multivariate logistic regression analysis was performed to identify independent risk factors for intra- or early postoperative complications. Out of 120 randomized women, 103 (86%) remained for final analysis. Surgeons assessed the tissue quality similarity in cases with or without LET, representing no statistically significant differences concerning tissue perfusion, tissue atrophy, tissue consistency, difficulty of dissection and regular pelvic anatomy. Regarding pre-treatment, the rating of the surgeon correlated significantly with LET (r = 0.043), meaning a correct assumption of the surgeon. Operative time, intraoperative blood loss, occurrence of intraoperative complications, total length of stay, frequent use of analgesics and rate of readmission did not significantly differ between LET and placebo pre-treatment. The rate of defined postoperative complications and use of antibiotics was significantly more frequent in patients without LET ( p = 0.045 and p = 0.003). Tissue quality was similarly assessed in cases with or without local estrogen pre-treatment, but it seems that LET prior to prolapse surgery may improve vaginal health as well as tissue-healing processes, protecting these patients from early postoperative complications.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence.
- Record: found
- Abstract: found
- Article: not found