- Record: found
- Abstract: found
- Article: found
Pulmonary Embolism and Coexisting Deep Vein Thrombosis: A Detrimental Association?
Read this article at
Abstract
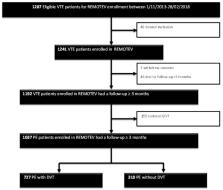
Background: The prognostic significance of coexisting deep vein thrombosis (DVT) in acute pulmonary embolism (PE) is controversial. This study aimed to provide routine patient care data on the impact of this association on PE severity and 3-month outcomes in a population presenting with symptomatic venous thromboembolism (VTE) from the REMOTEV registry. Methods and Results: REMOTEV is a prospective, non-interventional study of patients with acute symptomatic VTE, treated with direct oral anticoagulants (DOACs) or standard anticoagulation (vitamin K antagonists (VKA) or parenteral heparin/fondaparinux alone) for at least 3 months. From 1 November 2013 to 28 February 2018, among 1241 consecutive patients included, 1192 had a follow-up of at least 3 months and, among them, 1037 had PE with (727) or without DVT (310). The median age was 69 (55–80, 25th–75th percentiles). Patients with PE-associated DVT had more severe forms of PE ( p < 0.0001) and, when DVT was present, proximal location was significantly correlated to PE severity ( p < 0.01). However, no difference in all-cause mortality rate (hazard ratio (HR) 1.36 (CI 95% 0.69–2.92)), nor in the composite criterion of all-cause mortality and recurrence rate (HR 1.56 (CI 95% 0.83–3.10)) was noted at 3 months of follow-up. Conclusion: In REMOTEV, coexisting DVT was associated with a higher severity of PE, with no impact on short-term prognosis.
Related collections
Most cited references21
- Record: found
- Abstract: not found
- Article: not found
2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism.
- Record: found
- Abstract: found
- Article: not found
Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER)
- Record: found
- Abstract: found
- Article: not found