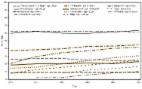
Problem/Condition Overall, the prevalence of illness attributable to vaccine-preventable diseases is greater among adults than among children. Adults are recommended to receive vaccinations based on their age, underlying medical conditions, lifestyle, prior vaccinations, and other considerations. Updated vaccination recommendations from CDC are published annually in the U.S. Adult Immunization Schedule. Despite longstanding recommendations for use of many vaccines, vaccination coverage among U.S. adults is low. Period Covered August 2014–June 2015 (for influenza vaccination) and January–December 2015 (for pneumococcal, tetanus and diphtheria [Td] and tetanus and diphtheria with acellular pertussis [Tdap], hepatitis A, hepatitis B, herpes zoster, and human papillomavirus [HPV] vaccination). Description of System The National Health Interview Survey (NHIS) is a continuous, cross-sectional national household survey of the noninstitutionalized U.S. civilian population. In-person interviews are conducted throughout the year in a probability sample of households, and NHIS data are compiled and released annually. The survey objective is to monitor the health of the U.S. population and provide estimates of health indicators, health care use and access, and health-related behaviors. Results Compared with data from the 2014 NHIS, increases in vaccination coverage occurred for influenza vaccine among adults aged ≥19 years (a 1.6 percentage point increase compared with the 2013–14 season to 44.8%), pneumococcal vaccine among adults aged 19–64 years at increased risk for pneumococcal disease (a 2.8 percentage point increase to 23.0%), Tdap vaccine among adults aged ≥19 years and adults aged 19–64 years (a 3.1 percentage point and 3.3 percentage point increase to 23.1% and to 24.7%, respectively), herpes zoster vaccine among adults aged ≥60 years and adults aged ≥65 years (a 2.7 percentage point and 3.2 percentage point increase to 30.6% and to 34.2%, respectively), and hepatitis B vaccine among health care personnel (HCP) aged ≥19 years (a 4.1 percentage point increase to 64.7%). Herpes zoster vaccination coverage in 2015 met the Healthy People 2020 target of 30%. Aside from these modest improvements, vaccination coverage among adults in 2015 was similar to estimates from 2014. Racial/ethnic differences in coverage persisted for all seven vaccines, with higher coverage generally for whites compared with most other groups. Adults without health insurance reported receipt of influenza vaccine (all age groups), pneumococcal vaccine (adults aged 19–64 years at increased risk), Td vaccine (adults aged ≥19 years, 19–64 years, and 50–64 years), Tdap vaccine (adults aged ≥19 years and 19–64 years), hepatitis A vaccine (adults aged ≥19 years overall and among travelers), hepatitis B vaccine (adults aged ≥19 years, 19–49 years, and among travelers), herpes zoster vaccine (adults aged ≥60 years), and HPV vaccine (males and females aged 19–26 years) less often than those with health insurance. Adults who reported having a usual place for health care generally reported receipt of recommended vaccinations more often than those who did not have such a place, regardless of whether they had health insurance. Vaccination coverage was higher among adults reporting one or more physician contacts in the past year compared with those who had not visited a physician in the past year, regardless of whether they had health insurance. Even among adults who had health insurance and ≥10 physician contacts within the past year, depending on the vaccine, 18.2%–85.6% reported not having received vaccinations that were recommended either for all persons or for those with specific indications. Overall, vaccination coverage among U.S.-born adults was higher than that among foreign-born adults, with few exceptions (influenza vaccination [adults aged 19–49 years and 50–64 years], hepatitis A vaccination [adults aged ≥19 years], and hepatitis B vaccination [adults aged ≥19 years with diabetes or chronic liver conditions]). Interpretation Coverage for all vaccines for adults remained low but modest gains occurred in vaccination coverage for influenza (adults aged ≥19 years), pneumococcal (adults aged 19–64 years with increased risk), Tdap (adults aged ≥19 years and adults aged 19–64 years), herpes zoster (adults aged ≥60 years and ≥65 years), and hepatitis B (HCP aged ≥19 years); coverage for other vaccines and groups with vaccination indications did not improve. The 30% Healthy People 2020 target for herpes zoster vaccination was met. Racial/ethnic disparities persisted for routinely recommended adult vaccines. Missed opportunities to vaccinate remained. Although having health insurance coverage and a usual place for health care were associated with higher vaccination coverage, these factors alone were not associated with optimal adult vaccination coverage. HPV vaccination coverage for males and females has increased since CDC recommended vaccination to prevent cancers caused by HPV, but many adolescents and young adults remained unvaccinated. Public Health Actions Assessing factors associated with low coverage rates and disparities in vaccination is important for implementing strategies to improve vaccination coverage. Evidence-based practices that have been demonstrated to improve vaccination coverage should be used. These practices include assessment of patients’ vaccination indications by health care providers and routine recommendation and offer of needed vaccines to adults, implementation of reminder-recall systems, use of standing-order programs for vaccination, and assessment of practice-level vaccination rates with feedback to staff members. For vaccination coverage to be improved among those who reported lower coverage rates of recommended adult vaccines, efforts also are needed to identify adults who do not have a regular provider or insurance and who report fewer health care visits.