- Record: found
- Abstract: found
- Article: found
Hospital mortality and prognostic factors in critically ill patients with acute kidney injury and cancer undergoing continuous renal replacement therapy
Read this article at
Abstract
Background
Whether continuous renal replacement therapy (CRRT) should be applied to critically ill patients with both acute kidney injury (AKI) and cancer remains controversial because of poor expected outcomes. The present study determined prognostic factors for all-cause in-hospital mortality in patients with AKI and cancer undergoing CRRT.
Methods
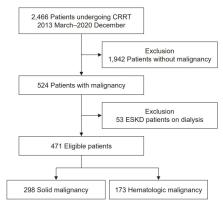
We included 471 patients with AKI and cancer who underwent CRRT at the intensive care unit of a Korean tertiary hospital from 2013 to 2020, and classified them by malignancy type. The primary outcomes were 28-day all-cause mortality rate and prognostic factors for in-hospital mortality. The secondary outcome was renal replacement therapy (RRT) dependency at hospital discharge.
Results
The 28-day mortality rates were 58.8% and 82% in the solid and hematologic malignancy groups, respectively. Body mass index (BMI), presence of oliguria, Sequential Organ Failure Assessment (SOFA) score, and albumin level were common predictors of 28-day mortality in the solid and hematologic malignancy groups. A high heart rate and the presence of severe acidosis were prognostic factors only in the solid malignancy group. Among the survivors, the proportion with RRT dependency was 25.0% and 33.3% in the solid and hematologic malignancy groups, respectively.
Conclusion
The 28-day mortality rate of cancer patients with AKI undergoing CRRT was high in both the solid and hematologic malignancy groups. BMI, presence of oliguria, SOFA score, and albumin level were common predictors of 28-day mortality in the solid and hematologic malignancy groups, but a high heart rate and severe acidosis were prognostic factors only in the solid malignancy group.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
APACHE II: a severity of disease classification system.
- Record: found
- Abstract: found
- Article: not found
SAPS 3—From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission
- Record: found
- Abstract: found
- Article: not found