- Record: found
- Abstract: found
- Article: found
The Diagnosis and Treatment of Acetabular Bone Loss in Revision Hip Arthroplasty: An International Consensus Symposium

Read this article at
Abstract
Despite growing evidence supporting the evaluation, classification, and treatment of acetabular bone loss in revision hip replacement, advancements have not been systematically incorporated into a single document, and therefore, a comprehensive review of the treatment of severe acetabular bone loss is needed. The Stavros Niarchos Foundation Complex Joint Reconstruction Center at Hospital for Special Surgery held an Acetabular Bone Loss Symposium on June 21, 2019, to answer the following questions: What are the trends, emerging technologies, and areas of future research related to the evaluation and management of acetabular bone loss in revision hip replacement? What constitutes the optimal workup and management strategies for acetabular bone loss? The 36 international experts convened were divided into groups, each assigned to discuss 1 of 4 topics: (1) preoperative planning and postoperative assessment; (2) implant selection, management of osteolysis, and management of massive bone loss; (3) the treatment challenges of pelvic discontinuity, periprosthetic joint infection, instability, and poor bone biology; and (4) the principles of reconstruction and classification of acetabular bone loss. Each group came to consensus, when possible, based on an extensive literature review. This document provides an overview of these 4 areas, the consensus each group arrived at, and directions for future research.
Related collections
Most cited references269
- Record: found
- Abstract: found
- Article: found
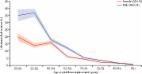
The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study
- Record: found
- Abstract: found
- Article: not found
Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation.
- Record: found
- Abstract: found
- Article: not found
