- Record: found
- Abstract: found
- Article: found
Effects of active vitamin D on insulin resistance and islet β-cell function in non-diabetic chronic kidney disease patients: a randomized controlled study
Read this article at
Abstract
Purpose
The purpose of the study is to observe the effects of active vitamin D supplementation on insulin resistance and islet β-cell function (HOMA-β) in patients with non-diabetic chronic kidney disease (NDCKD).
Methods
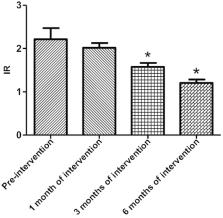
A total of 134 patients with NDCKD who met the inclusion criteria were enrolled in the prospective controlled study and categorized as such: 60 patients in the non-dialysis (ND) group; 36, hemodialysis (HD) group; and 38, peritoneal dialysis (PD) group. Each group was divided into two equal-numbered subgroups for vitamin D supplementation. Those in the experimental subgroups received calcitriol 0.5 ug/day orally, and were followed-up for 6 months. A total of 117 patients were followed-up, including 57 patients in the ND group; 29, HD group; and 31, PD group. Changes in the insulin resistance index (HOMA-IR) and HOMA-β index were calculated and compared at the time of enrollment and after 1, 3, and 6 months of intervention.
Results
(1) Mean HOMA-IR value: In the ND group, mean HOMA-IR value of the experimental group significantly decreased compared with that of the control group after 3 months of intervention ( P = 0.02). In the HD and PD groups, there was no statistical difference between the experimental and control groups ( P > 0.05). (2) Mean HOMA-β index: In the ND group, mean HOMA-β index of the experimental group was higher than that of the control group after 1 month of active vitamin D treatment ( P = 0.03), and, with an extended intervention time, the index gradually increased ( P < 0.001). In the HD group, mean HOMA-β index of the experimental group was higher than that of the control group after 3 months of active vitamin D treatment ( P = 0.01). Among PD patients, mean HOMA-β index of the patients in the experimental group was higher than that of the control group after 6 months of active vitamin D treatment ( P = 0.02).
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Vitamin D Switches BAF Complexes to Protect β Cells
- Record: found
- Abstract: found
- Article: not found
Insulin resistance and hyperinsulinemia are already present in patients with incipient renal disease.
- Record: found
- Abstract: found
- Article: not found