- Record: found
- Abstract: found
- Article: found
Applying a Health Network approach to translate evidence-informed policy into practice: A review and case study on musculoskeletal health
Read this article at
Abstract
Background
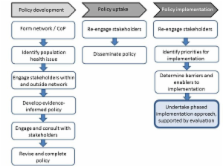
While translation of evidence into health policy and practice is recognised as critical to optimising health system performance and health-related outcomes for consumers, mechanisms to effectively achieve these goals are neither well understood, nor widely communicated. Health Networks represent a framework which offers a possible solution to this dilemma, particularly in light of emerging evidence regarding the importance of establishing relationships between stakeholders and identifying clinical leaders to drive evidence integration and translation into policy. This is particularly important for service delivery related to chronic diseases. In Western Australia (WA), disease and population-specific Health Networks are comprised of cross-discipline stakeholders who work collaboratively to develop evidence-informed policies and drive their implementation. Since establishment of the Health Networks in WA, over 50 evidence-informed Models of Care (MoCs) have been produced across 18 condition or population-focused Networks. The aim of this paper is to provide an overview of the Health Network framework in facilitating the translation of evidence into policy and practice with a particular focus on musculoskeletal health.
Case presentation
A review of activities of the WA Musculoskeletal Health Network was undertaken, focussing on outcomes and the processes used to achieve them in the context of: development of policy, procurement of funding, stakeholder engagement, publications, and projects undertaken by the Network which aligned to implementation of MoCs.
The Musculoskeletal Health Network has developed four MoCs which reflect Australian National Health Priority Areas. Establishment of community-based services for consumers with musculoskeletal health conditions is a key recommendation from these MoCs. Through mapping barriers and enablers to policy implementation, working groups, led by local clinical leaders and supported by the broader Network and government officers, have undertaken a range of integrated projects, such as the establishment of a community-based, multidisciplinary rheumatology service. The success of these projects has been contingent on developing relationships between key stakeholders across the health system.
Conclusions
In WA, Networks have provided a sustainable mechanism to meaningfully engage consumers, carers, clinicians and other stakeholders; provided a forum to exchange ideas, information and evidence; and collaboratively plan and deliver evidence-based and contextually-appropriate health system improvements for consumers.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures.
- Record: found
- Abstract: found
- Article: not found
A randomized trial of vertebroplasty for osteoporotic spinal fractures.
- Record: found
- Abstract: found
- Article: not found