- Record: found
- Abstract: found
- Article: found
Association of self-rated health with multimorbidity, chronic disease and psychosocial factors in a large middle-aged and older cohort from general practice: a cross-sectional study
Read this article at
Abstract
Background
The prevalence of coexisting chronic conditions (multimorbidity) is rising. Disease labels, however, give little information about impact on subjective health and personal illness experience. We aim to examine the strength of association of single and multimorbid physical chronic diseases with self-rated health in a middle-aged and older population in England, and to determine whether any association is mediated by depression and other psychosocial factors.
Methods
25 268 individuals aged 39 to 79 years recruited from general practice registers in the European Prospective Investigation of Cancer (EPIC-Norfolk) study, completed a survey including self-rated health, psychosocial function and presence of common physical chronic conditions (cancer, stroke, heart attack, diabetes, asthma/bronchitis and arthritis). Logistic regression models determined odds of “moderate/poor” compared to “good/excellent” health by condition and number of conditions adjusting for psychosocial measures.
Results
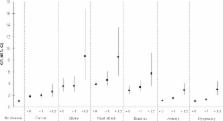
One-third (8252) reported one, around 7.5% (1899) two, and around 1% (194) three or more conditions. Odds of “moderate/poor” self-rated health worsened with increasing number of conditions (one (OR = 1.3(1.2–1.4)) versus three or more (OR = 3.4(2.3–5.1)), and were highest where there was comorbidity with stroke (OR = 8.7(4.6–16.7)) or heart attack (OR = 8.5(5.3–13.6)). Psychosocial measures did not explain the association between chronic diseases and multimorbidity with self-rated health.The relationship of multimorbidity with self-rated health was particularly strong in men compared to women (three or more conditions: men (OR = 5.2(3.0–8.9)), women OR = 2.1(1.1–3.9)).
Conclusions
Self-rated health provides a simple, integrative patient-centred assessment for evaluation of illness in the context of multiple chronic disease diagnoses. Those registering in general practice in particular men with three or more diseases or those with cardiovascular comorbidities and with poorer self-rated health may warrant further assessment and intervention to improve their physical and subjective health.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
The development of a comorbidity index with physical function as the outcome.
- Record: found
- Abstract: found
- Article: not found