- Record: found
- Abstract: found
- Article: found
Weight Gain in Early Life Predicts Risk of Islet Autoimmunity in Children With a First-Degree Relative With Type 1 Diabetes
Read this article at
Abstract
OBJECTIVE—In a prospective birth cohort study, we followed infants who had a first-degree relative with type 1 diabetes to investigate the relationship between early growth and infant feeding and the risk of islet autoimmunity.
RESEARCH DESIGN AND METHODS—Infants with a first-degree relative with type 1 diabetes were identified during their mother's pregnancy. Dietary intake was recorded prospectively to determine duration of breast-feeding and age at introduction of cow's milk protein, cereals, meat, fruit, and vegetables. At 6-month reviews, length (or height) and weight, antibodies to insulin, GAD65, the tyrosine phosphatase-like insulinoma antigen, and tissue transglutaminase were measured. Islet autoimmunity was defined as persistent elevation of one or more islet antibodies at consecutive 6-month intervals, including the most recent measure, and was the primary outcome measure.
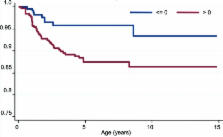
RESULTS—Follow-up of 548 subjects for 5.7 ± 3.2 years identified 46 children with islet autoimmunity. Weight z score and BMI z score were continuous predictors of risk of islet autoimmunity (adjusted hazard ratios 1.43 [95% CI 1.10–1.84], P = 0.007, and 1.29 [1.01–1.67], P = 0.04, respectively). The risk of islet autoimmunity was greater in subjects with weight z score >0 than in those with weight z score ≤0 over time (2.61 [1.26–5.44], P = 0.01). Weight z score and BMI z score at 2 years and change in weight z score between birth and 2 years, but not dietary intake, also predicted risk of islet autoimmunity.
CONCLUSIONS—Weight gain in early life predicts risk of islet autoimmunity in children with a first-degree relative with type 1 diabetes.
Related collections
Most cited references15
- Record: found
- Abstract: not found
- Article: not found
Diabetes
- Record: found
- Abstract: found
- Article: not found
Early infant feeding and risk of developing type 1 diabetes-associated autoantibodies.
- Record: found
- Abstract: found
- Article: not found