- Record: found
- Abstract: found
- Article: found
Dexamethasone intravitreal implant in the treatment of diabetic macular edema
Read this article at
Abstract
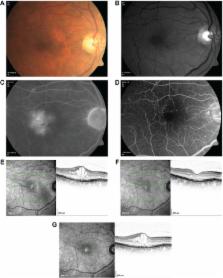
Diabetic macular edema (DME) resembles a chronic, low-grade inflammatory reaction, and is characterized by blood–retinal barrier (BRB) breakdown and retinal capillary leakage. Corticosteroids are of therapeutic benefit because of their anti-inflammatory, antiangiogenic, and BRB-stabilizing properties. Delivery modes include periocular and intravitreal (via pars plana) injection. To offset the short intravitreal half-life of corticosteroid solutions (~3 hours) and the need for frequent intravitreal injections, sustained-release intravitreal corticosteroid implants have been developed. Dexamethasone intravitreal implant provides retinal drug delivery for ≤6 months and recently has been approved for use in the treatment of DME. Pooled findings (n=1,048) from two large-scale, randomized Phase III trials indicated that dexamethasone intravitreal implant (0.35 mg and 0.7 mg) administered at ≥6-month intervals produced sustained improvements in best-corrected visual acuity (BCVA) and macular edema. Significantly more patients showed a ≥15-letter gain in BCVA at 3 years with dexamethasone intravitreal implant 0.35 mg and 0.7 mg than with sham injection (18.4% and 22.2% vs 12.0%). Anatomical assessments showed rapid and sustained reductions in macular edema and slowing of retinopathy progression. Phase II study findings suggest that dexamethasone intravitreal implant is effective in focal, cystoid, and diffuse DME, in vitrectomized eyes, and in combination with laser therapy. Ocular complications of dexamethasone intravitreal implant in Phase III trials included cataract-related events (66.0% in phakic patients), intraocular pressure elevation ≥25 mmHg (29.7%), conjunctival hemorrhage (23.5%), vitreous hemorrhage (10.0%), macular fibrosis (8.3%), conjunctival hyperemia (7.2%), eye pain (6.1%), vitreous detachment (5.8%), and dry eye (5.8%); injection-related complications (eg, retinal tear/detachment, vitreous loss, endophthalmitis) were infrequent (<2%). Dexamethasone intravitreal implant offers a viable treatment option for DME, especially in cases that are persistent or treatment (anti-vascular endothelial growth factor/laser) refractory.
Related collections
Most cited references73
- Record: found
- Abstract: found
- Article: not found
A central role for inflammation in the pathogenesis of diabetic retinopathy.
- Record: found
- Abstract: found
- Article: not found
Diabetic retinopathy: seeing beyond glucose-induced microvascular disease.
- Record: found
- Abstract: found
- Article: not found