- Record: found
- Abstract: found
- Article: found
Pulmonary embolism presenting with itinerant chest pain and migratory pleural effusion : A case report
Read this article at
Abstract
Introduction:
Pulmonary embolism (PE) presents with complex clinical manifestations ranging from asymptomatic to chest pain, hemoptysis, syncope, shock, or sudden death. To the authors’ knowledge, itinerant chest pain has not been reported as sign or symptom of PE.
Case presentation:
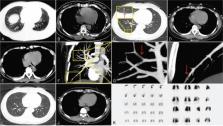
A 41-year-old woman presenting with left chest pain, no hemoptysis, or breathing difficulties. The chest pain was more severe on deep inspiration. Chest computed tomography (CT) and ultrasound imaging showed left pleural effusion. After antibiotic treatment, the left chest pain was alleviated, but a similar pain appeared in the right chest. Electrocardiogram, blood gas analysis, echocardiography, and D-dimer levels were unremarkable. Chest CT showed right pleural effusion. A CT pulmonary angiography (CTPA) unexpectedly revealed a PE in the right pulmonary artery. The patient was administered anticoagulant therapy and made a complete recovery.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer.
- Record: found
- Abstract: found
- Article: not found
The diagnosis of pleural effusions.
- Record: found
- Abstract: found
- Article: not found