- Record: found
- Abstract: found
- Article: found
Impact of Intra-Articular Local Anesthesia Infiltration versus Femoral Nerve Block for Postoperative Pain Management in Total Knee Arthroplasty
Read this article at
Abstract
Background:
Postoperative pain relief after total knee arthroplasty (TKA) can be attained by using several techniques such as intravenous analgesia, epidural analgesia, and peripheral nerve blocks that include femoral nerve and saphenous nerve. Several authors recommended intra-articular injection of local anesthetic (IALA) as a part of multimodal analgesia regimens for TKA instead of other techniques.
Aims:
The present study compares IALA technique efficacy with single-shot femoral nerve block (FNB) as part of multimodal analgesia regimen in TKA patients for postoperative pain management.
Subjects and Methods:
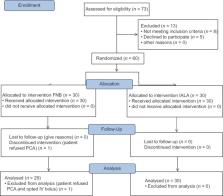
We recruited a total of 60 patients scheduled for unilateral total knee replacement under spinal anesthesia. Subjects were allocated randomly into two groups FNB and IALA receiving ultrasound-guided FNB and Intra-articular local anesthesia and morphine mix infiltration, respectively. Twenty-four hour postoperative morphine consumption through patient-controlled analgesia was the primary outcome measure in our study. Secondary outcome measures were pain scores, nausea and vomiting.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients.

- Record: found
- Abstract: found
- Article: found
Why still in hospital after fast-track hip and knee arthroplasty?
- Record: found
- Abstract: found
- Article: not found