- Record: found
- Abstract: found
- Article: found
Comparative Evaluation of Crystalloid Resuscitation Rate in a Human Model of Compensated Haemorrhagic Shock
Read this article at
ABSTRACT
Methods:
We performed a randomized crossover pilot study in a healthy volunteer model of compensated haemorrhagic shock. Following venesection of 15 mL/kg of blood, participants were randomized to 20 mL/kg of crystalloid over 10 min (FAST treatment) or 30 min (SLOW treatment). The primary end point was oxygen delivery (DO 2). Secondary end points included pressure and flow-based haemodynamic variables, blood volume expansion, and clinical biochemistry.
Results:
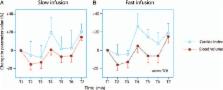
Nine normotensive healthy adult volunteers participated. No significant differences were observed in DO 2 and biochemical variables between the SLOW and FAST groups. Blood volume was reduced by 16% following venesection, with a corresponding 5% reduction in cardiac index (CI) ( P < 0.001). Immediately following resuscitation the increase in blood volume corresponded to 54% of the infused volume under FAST treatment and 69% of the infused volume under SLOW treatment ( P = 0.03). This blood volume expansion attenuated with time to 24% and 25% of the infused volume 30 min postinfusion. During fluid resuscitation, blood pressure was higher under FAST treatment. However, CI paradoxically decreased in most participants during the resuscitation phase; a finding not observed under SLOW treatment.
Conclusion:
FAST or SLOW fluid resuscitation had no significant impact on DO 2 between treatment groups. In both groups, changes in CI and blood pressure did not reflect the magnitude of intravascular blood volume deficit. Crystalloid resuscitation expanded intravascular blood volume by approximately 25%.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries.
- Record: found
- Abstract: found
- Article: not found
Nexfin noninvasive continuous blood pressure validated against Riva-Rocci/Korotkoff.
- Record: found
- Abstract: found
- Article: not found