- Record: found
- Abstract: found
- Article: found
PrePex Male Circumcision: Follow-Up and Outcomes during the First Two Years of Implementation at the Rwanda Military Hospital

Read this article at
Abstract
Background
PrePex Male Circumcision (MC) has been demonstrated as an effective and scalable strategy to prevent HIV infection in low- and middle-income countries. This study describes the follow-up and outcomes of clients who underwent PrePex MC between January 2011 and December 2012 with weekly follow-up at the Rwanda Military Hospital, the first national hospital in Rwanda to adopt PrePex.
Methods
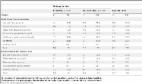
Data on570 clients age 21 to 54 were extracted from patient records. We compared socio-demographic and clinical characteristics, the operator's qualification, HIV status, pain before and after device removal, urological status, device size and follow-up time between clients who were formally discharged and those who defaulted. We reported bivariate associations between each covariate and discharge status, number of people with adverse events by discharge status, and time to formal discharge or defaulting using life table methods. Data were entered into Epidata and analyzed with Stata v13.
Results
Among study participants, 96.5% were circumcised by non-physician operators, 85.4%were under 30years, 98.9% were HIV-negative and 97.9% were without any urological problems that could delay the healing time. Most (70.7%) defaulted before formal discharge. Pain before (p<0.001) and after PrePex device removal (p = 0.001) were associated with discharge status, although very few cases were reported, and pain was more commonly missing among defaulters. Twenty-seven adverse events were reported (7 formally discharged, 20 defaulters). Median follow-up time was seven weeks among formally discharged and six weeks among defaulters (p<0.001).
Conclusion
Given that all socio-demographic and most clinical characteristics were not associated with defaulting, we hypothesize that clients stopped returning once they determined they were healed. We recommend less frequent follow-up protocols to encourage clinical visits until formal discharge. Based on these results and recommendations, we believe PrePex MC is a practical circumcision strategy in Rwanda and in sub-Saharan Africa.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Male circumcision for HIV prevention in sub-Saharan Africa: who, what and when?
- Record: found
- Abstract: found
- Article: not found
HIV prevention: male circumcision comparison between a nonsurgical device to a surgical technique in resource-limited settings: a prospective, randomized, nonmasked trial.
- Record: found
- Abstract: found
- Article: found