- Record: found
- Abstract: found
- Article: found
Anemia in Ugandan pregnant women: a cross-sectional, systematic review and meta-analysis study
Read this article at
Abstract
Background
Anemia in pregnancy represents a global public health concern due to wide ranging maternal and neonatal adverse outcomes in all peripartum periods. We estimated the prevalence and factors associated with anemia in pregnancy at a national obstetrics and gynecology referral hospital in Uganda and in addition performed a systematic review and meta-analysis of the overall burden of anemia in pregnancy in Uganda.
Methods
We conducted a cross-sectional study among 263 pregnant women attending the antenatal care clinic of Kawempe National Referral Hospital, Kampala, Uganda, in September 2020. Anemia in pregnancy was defined as a hemoglobin level of < 11.0 g/dl and microcytosis as a mean corpuscular volume (MCV) of < 76 fL. We also performed a systematic review (PROSPERO Registration ID : CRD42020213001) and meta-analysis of studies indexed on MEDLINE, Embase, African Journal Online, ClinicalTrials.gov, ICTRP, and the Cochrane Library of systematic review between 1 January 2000 and 31 September 2020 reporting on the prevalence of anemia in pregnancy in Uganda.
Results
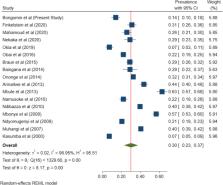
The prevalence of anemia was 14.1% ( n= 37) (95%CI 10.4–18.8), of whom 21 (56.8%) had microcytic anemia. All cases of anemia occurred in the second or third trimester of pregnancy and none were severe. However, women with anemia had significantly lower MCV (75.1 vs. 80.2 fL, p<0.0001) and anthropometric measurements, such as weight (63.3 vs. 68.9kg; p=0.008), body mass index (25.2 vs. 27.3, p=0.013), hip (98.5 vs. 103.8 cm, p=0.002), and waist (91.1 vs. 95.1 cm, p=0.027) circumferences and mean systolic blood pressure (BP) (118 vs 125 mmHg, p=0.014). Additionally, most had BP within the normal range (59.5% vs. 34.1%, p=0.023). The comparison meta-analysis of pooled data from 17 published studies of anemia in pregnancy in Uganda, which had a total of 14,410 pregnant mothers, revealed a prevalence of 30% (95% CI 23–37).
Conclusions
Despite our study having a lower prevalence compared to other studies in Uganda, these findings further confirm that anemia in pregnancy is still of public health significance and is likely to have nutritional causes, requiring targeted interventions. A larger study would be necessary to demonstrate potential use of basic clinical parameters such as weight or blood pressure as screening predictors for anemia in pregnancy.
Related collections
Most cited references41
- Record: found
- Abstract: not found
- Article: not found
Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation
- Record: found
- Abstract: found
- Article: not found