- Record: found
- Abstract: found
- Article: found
Effects of Berries Consumption on Cardiovascular Risk Factors: A Meta-analysis with Trial Sequential Analysis of Randomized Controlled Trials
Read this article at
Abstract
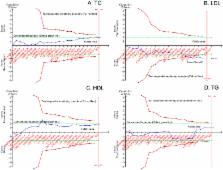
The effects of berries consumption on cardiovascular disease (CVD) risk factors have not been systematically examined. Here, we aimed to conduct a meta-analysis with trial sequential analysis to estimate the effect of berries consumption on CVD risk factors. PubMed, Embase, and CENTRAL were searched for randomized controlled trials (RCTs) that regarding the effects of berries consumption in either healthy participants or patients with CVD. Twenty-two eligible RCTs representing 1,251 subjects were enrolled. The pooled result showed that berries consumption significantly lowered the low density lipoprotein (LDL)-cholesterol [weighted mean difference (WMD), −0.21 mmol/L; 95% confidence interval (CI), −0.34 to −0.07; P = 0.003], systolic blood pressure (SBP) (WMD, −2.72 mmHg; 95% CI, −5.32 to −0.12; P = 0.04), fasting glucose (WMD, −0.10 mmol/L; 95% CI, −0.17 to −0.03; P = 0.004), body mass index (BMI) (WMD, −0.36 kg/m 2; 95% CI, −0.54 to −0.18, P < 0.00001), Hemoglobin A1c (HbA1c) (WMD, −0.20%; 95% CI, −0.39 to −0.01; P = 0.04) and tumor necrosis factor-α (TNF-α) (WMD, −0.99 ρg/mL; 95% CI, −1.96 to −0.02; P = 0.04). However, no significant changes were seen in other markers. The current evidence suggests that berries consumption might be utilized as a possible new effective and safe supplementary option to better prevent and control CVD in humans.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies.
- Record: found
- Abstract: not found
- Article: not found
2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.
- Record: found
- Abstract: found
- Article: not found