- Record: found
- Abstract: found
- Article: found
Poster 200: High Prevalence of Abnormal Imaging Findings in Clinically Asymptomatic Siblings Of JOCD Patients On 3T Knee MRI
Read this article at
Abstract
Objectives:
Endochondral ossification is a skeletal developmental process in children by which the embryonic cartilaginous model of bones undergoes gradual ossification over time until skeletal maturity is reached. Juvenile Osteochondritis Dissecans (JOCD) is a developmental disease characterized by focal areas of chondronecrosis within the epiphyseal cartilage and subsequent delay of the ossification front. JOCD lesions can become loose bodies and lead to premature Osteoarthritis. The etiology of JOCD is not yet well understood, however, there is mounting evidence of a genetic predisposition. Recently, positive familial history, including familial OCD and a genome-wide association study in humans identified genetic loci related to juvenile OCD. In this longitudinal pilot study, we examined siblings of JOCD patients utilizing clinical 3T MRI data to evaluate morphological integrity of the epiphyseal cartilage and the advancing ossification front in the distal femoral condyles in bilateral knees. We hypothesized that asymptomatic, clinically “silent” JOCD lesions could be detected in young siblings of patients affected by JOCD.
Methods:
In this longitudinal study, 44 MRI datasets from seven skeletally immature participants with no clinical symptoms (7 siblings of JOCD patients; 3 females; 12 bilateral knees; average age at first visit=8.7 years; range=6-10 years) were evaluated. This study was approved by the institutional review board and informed consent was obtained. All images were acquired at 3T MRI system with a 1Tx/15Rx knee coil. Sagittal PD-weighted TSE images without fat suppression (TR/TE = 3900/40 ms, resolution = 0.36x0.36 mm 2, scanning time = 1min:49s) and with fat suppression (TR/TE = 3530/40 ms, resolution = 0.36x0.36 mm 2, scanning time = 3min:46s) were acquired bilaterally at first visit and at multiple MRI follow-up studies ranging from 6-21 months. The images were reviewed by an experienced musculoskeletal radiologist using the following MRI criteria: (i) integrity of the ossification front; (ii) presence/absence of bone marrow edema; (iii) intact/disrupted secondary physis; and (iv) T2 hyperintensity in epiphyseal cartilage.
Results:
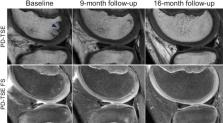
Five of seven participants (71%) met at least one of the MRI criteria defining a JOCD lesion. Six of the seven participants (86%) had an irregular ossification front at the distal aspect of the medial and/or lateral femoral epicondyles, focal areas of T2 hyperintensities in the epiphyseal cartilage, and a disrupted secondary physis. Of the 13 imaged knees, two knees (both lateral and medial epicondyle) from the same participant and two knees (only lateral epicondyle) had no abnormal MRI findings (= 6 normal epicondyles). Abnormal findings in the medial and lateral epicondyles of the remaining bilateral knees resolved over time in 11 epicondyles (Fig. 1), whereas in the remaining 9 epicondyles the abnormal findings persisted or progressed (Fig. 2).
Conclusions:
The most important finding of this pilot study is the high prevalence (6 out of 7, 86%) of morphological changes during skeletal development in this group of first-degree relatives of JOCD patients. Furthermore, 71% (5 out of 6) of participants met the imaging criteria for early JOCD lesions at least at one time point during the study without developing any clinical symptoms. There is mounting evidence of a genetic contribution to the etiology of JOCD. In the literature, so called ossification variants are considered morphological variants of bone shape with an overall prevalence of 12% and are believed to resolve naturally over time. While 55% of the epicondyles with abnormalities in the ossification front in our cohort resolved over time on MRI, during the course of this study – typically 8-21 months, the remaining 45% did not resolve or occurred at the last imaging time point with associated marrow edema and needed clinical surveillance. A high incidence of MRI abnormalities in the ossification front, epiphyseal cartilage and secondary physis in a clinically asymptomatic study group of first degree relatives of patients with JOCD supports the hypothesis a) that there is a strong genetic predisposition for this disease, b) clinically “silent” initial stages of the disease could be overlooked, challenging the common current understanding of normal physiologic “ossification variants”.

Sagittal PD-weighted TSE w/o fat-suppression (FS) of the lateral femoral condyle in a 10-year-old boy. The follow-up studies demonstrate complete resolution of the irregular ossification front (arrowhead), absence of bone marrow edema.
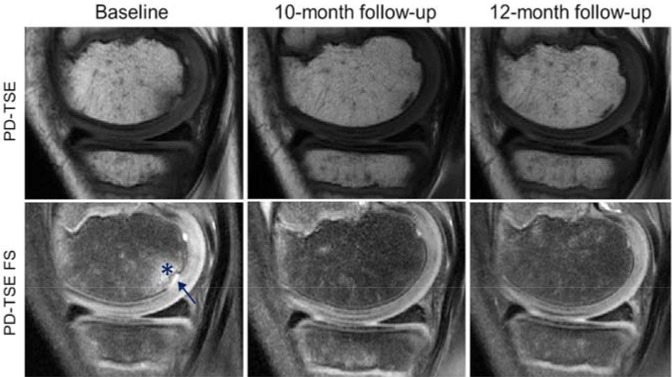
Sagittal PD-weighted TSE w/o fat-suppression (FS) of the lateral femoral condyle in a 10-year-old boy. The baseline study demonstrates a focal T2-hyperintense lesion (arrow) and a delayed ossification front with associated bone marrow edema (*) meeting the MR imaging criteria for an early JOCD lesion. The asymptomatic sibling was clinically surveilled and subsequent follow-up studies demonstrated resolution of the MR imaging findings.