- Record: found
- Abstract: found
- Article: found
Machine Learning of Infant Spontaneous Movements for the Early Prediction of Cerebral Palsy: A Multi-Site Cohort Study
Read this article at
Abstract
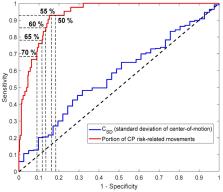
Background: Early identification of cerebral palsy (CP) during infancy will provide opportunities for early therapies and treatments. The aim of the present study was to present a novel machine-learning model, the Computer-based Infant Movement Assessment (CIMA) model, for clinically feasible early CP prediction based on infant video recordings. Methods: The CIMA model was designed to assess the proportion (%) of CP risk-related movements using a time–frequency decomposition of the movement trajectories of the infant’s body parts. The CIMA model was developed and tested on video recordings from a cohort of 377 high-risk infants at 9–15 weeks corrected age to predict CP status and motor function (ambulatory vs. non-ambulatory) at mean 3.7 years age. The performance of the model was compared with results of the general movement assessment (GMA) and neonatal imaging. Results: The CIMA model had sensitivity (92.7%) and specificity (81.6%), which was comparable to observational GMA or neonatal cerebral imaging for the prediction of CP. Infants later found to have non-ambulatory CP had significantly more CP risk-related movements (median: 92.8%, p = 0.02) compared with those with ambulatory CP (median: 72.7%). Conclusion: The CIMA model may be a clinically feasible alternative to observational GMA.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
A report: the definition and classification of cerebral palsy April 2006.
- Record: found
- Abstract: found
- Article: not found
An update on the prevalence of cerebral palsy: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found