- Record: found
- Abstract: found
- Article: found
Impact of urbanisation and altitude on the incidence of, and risk factors for, hypertension
Read this article at
Abstract
Background
Most of the data regarding the burden of hypertension in low-income and middle-income countries comes from cross-sectional surveys instead of longitudinal studies. We estimated the incidence of, and risk factors for, hypertension in four study sites with different degree of urbanisation and altitude.
Methods
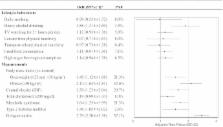
Data from the CRONICAS Cohort Study, conducted in urban, semiurban and rural areas in Peru, was used. An age-stratified and sex-stratified random sample of participants was taken from the most updated census available in each site. Hypertension was defined as systolic blood pressure ≥140 mm Hg, or diastolic blood pressure ≥90 mm Hg, or self-report physician diagnosis and current treatment. The exposures were study site and altitude as well as modifiable risk factors. Incidence, incidence rate ratios (IRRs), 95% CIs and population-attributable fractions (PAFs) were estimated using generalised linear models.
Results
Information from 3237 participants, mean age 55.8 (SD±12.7) years, 48.4% males, was analysed. Overall baseline prevalence of hypertension was 19.7% (95% CI 18.4% to 21.1%). A total of 375 new cases of hypertension were recorded, including 5266 person-years of follow-up, with an incidence of 7.12 (95% CI 6.44 to 7.88) per 100 person-years. Individuals from semiurban site were at higher risk of hypertension compared with highly urbanised areas (IRR=1.76; 95% CI 1.39 to 2.23); however, those from high-altitude sites had a reduced risk (IRR=0.74; 95% CI 0.58 to 0.95). Obesity was the leading risk factor for hypertension with a great variation according to study site with PAF ranging from 12.5% to 42.4%.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010
- Record: found
- Abstract: found
- Article: not found
National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants.
- Record: found
- Abstract: found
- Article: not found