- Record: found
- Abstract: found
- Article: found
Residual SYNTAX Score and One-Year Outcome in Elderly Patients With Acute Coronary Syndrome
Read this article at
Abstract
Background
The residual burden of coronary artery disease after percutaneous coronary intervention (PCI) has been associated with worse ischemic outcome. However, data are conflicting in elderly patients. The aim of our study was to verify the incremental value of the residual Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score (rSS) over clinical variables and baseline SYNTAX score (bSS) in predicting 1-year mortality or cardiovascular events.
Methods
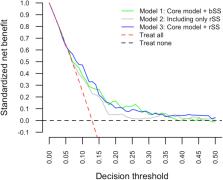
A post hoc analysis of data collected in the Elderly-ACS 2 multicenter randomized trial was performed. We included 630 patients aged > 75 years with multivessel coronary disease undergoing PCI for acute coronary syndrome (ACS). The primary outcome was a composite of death, recurrent myocardial infarction, and stroke at 1-year follow up. Change in c-statistic and standardized net benefit were used to evaluate the incremental value of the rSS.
Results
Event rates were significantly higher in patients with incomplete revascularization (rSS > 8). When the rSS was included in a core Cox regression model containing age, previous myocardial infarction, and ACS type, the hazard ratio for patients with score values > 8 was 2.47 (95% confidence interval, 1.51-4.06). However, the core model with rSS did not increase the c-statistic compared with the core model with the bSS (from 0.69 to 0.70) and gave little incremental value in the standardized net benefit.
Conclusions
In elderly patients with ACS with multivessel disease undergoing PCI, incomplete revascularization was associated with worse outcome at 1-year follow-up. However, there was no clear incremental value of the rSS in the prediction of 1-year adverse outcome compared with a model including clinical variables and bSS.
Résumé
Le fardeau résiduel de la coronaropathie après une intervention coronarienne percutanée (ICP) a été associé à de moins bons résultats sur le plan ischémique. Les données recueillies chez les patients âgés sont toutefois contradictoires. Cette étude avait donc pour objectif de valider la valeur ajoutée du score SYNTAX ( SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) résiduel (SSr) par rapport aux paramètres cliniques et au score SYNTAX initial (SSi) pour prédire la mortalité à 1 an et les manifestations cardiovasculaires.
Une analyse a posteriori des données de l’étude multicentrique avec répartition aléatoire Elderly-ACS 2 a été effectuée. Pour ce faire, 630 patients âgés de plus de 75 ans, atteints d’une coronaropathie multitronculaire et ayant subi une ICP pour traiter un syndrome coronarien aigu (SCA) ont été retenus. Le critère d’évaluation principal était composé du décès, de l’infarctus du myocarde récurrent et de l’accident vasculaire cérébral (AVC) au moment du suivi à 1 an. La variation de la statistique C et le bénéfice net normalisé ont servi à évaluer la valeur ajoutée du SSr.
Les manifestations étaient significativement plus fréquentes chez les patients dont la revascularisation était incomplète (SSr > 8). Lorsque le SSr a été pris en compte dans un modèle de régression de Cox de base ayant pour facteurs l’âge, les antécédents d’infarctus du myocarde et le type de SCA, le rapport des risques instantanés pour les patients ayant un score > 8 était de 2,47 (intervalle de confiance à 95 % : 1,51-4,06). L’intégration du SSr dans le modèle de base n’a toutefois pas donné lieu à une statistique C plus élevée que celle du SSi (0,70 vs 0,69) et conférait peu de valeur ajoutée sur le plan du bénéfice net normalisé.
Chez les patients âgés présentant un SCA et une atteinte multitronculaire, et subissant une ICP, la revascularisation incomplète a été associée à de moins bons résultats au moment du suivi à 1 an. Le SSr n’a toutefois pas été clairement associé à une valeur ajoutée pour prédire une issue défavorable à 1 an comparativement à un modèle reposant sur des paramètres cliniques et le SSi.
Related collections
Most cited references21
- Record: found
- Abstract: not found
- Article: not found
The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease.
- Record: found
- Abstract: found
- Article: not found
Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II.
- Record: found
- Abstract: found
- Article: not found