- Record: found
- Abstract: found
- Article: found
Febrile Neutropenia in Acute Leukemia. Epidemiology, Etiology, Pathophysiology and Treatment
Read this article at
Abstract
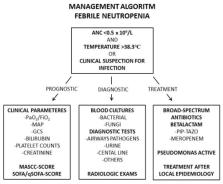
Acute leukemias are a group of aggressive malignant diseases associated with a high degree of morbidity and mortality. An important cause of both the latter is infectious complications. Patients with acute leukemia are highly susceptible to infectious diseases due to factors related to the disease itself, factors attributed to treatment, and specific individual risk factors in each patient. Patients with chemotherapy-induced neutropenia are at particularly high risk, and microbiological agents include viral, bacterial, and fungal agents. The etiology is often unknown in infectious complications, although adequate patient evaluation and sampling have diagnostic, prognostic and treatment-related consequences. Bacterial infections include a wide range of potential microbes, both Gram-negative and Gram-positive species, while fungal infections include both mold and yeast. A recurring problem is increasing resistance to antimicrobial agents, and in particular, this applies to extended-spectrum beta-lactamase resistance (ESBL), Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE) and even carbapenemase-producing Enterobacteriaceae (CPE). International guidelines for the treatment of sepsis in leukemia patients include the use of broad-spectrum Pseudomonas-acting antibiotics. However, one should implant the knowledge of local microbiological epidemiology and resistance conditions in treatment decisions. In this review, we discuss infectious diseases in acute leukemia with a major focus on febrile neutropenia and sepsis, and we problematize the diagnostic, prognostic, and therapeutic aspects of infectious complications in this patient group. Meticulously and thorough clinical and radiological examination combined with adequate microbiology samples are cornerstones of the examination. Diagnostic and prognostic evaluation includes patient review according to the multinational association for supportive care in cancer (MASCC) and sequential organ failure assessment (SOFA) scoring system. Antimicrobial treatments for important etiological agents are presented. The main challenge for reducing the spread of resistant microbes is to avoid unnecessary antibiotic treatment, but without giving to narrow treatment to the febrile neutropenic patient that reduce the prognosis.
Related collections
Most cited references130
- Record: found
- Abstract: found
- Article: not found
Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america.
- Record: found
- Abstract: found
- Article: not found
Time to Treatment and Mortality during Mandated Emergency Care for Sepsis.
- Record: found
- Abstract: not found
- Article: not found