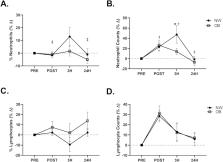
An ever-growing volume of peer-reviewed publications speaks to the recent and rapid growth in both scope and understanding of exercise immunology. Indeed, more than 95% of all peer-reviewed publications in exercise immunology (currently >2, 200 publications using search terms "exercise" and "immune") have been published since the formation of the International Society of Exercise and Immunology (ISEI) in 1989 (ISI Web of Knowledge). We recognise the epidemiological distinction between the generic term "physical activity" and the specific category of "exercise", which implies activity for a specific purpose such as improvement of physical condition or competition. Extreme physical activity of any type may have implications for the immune system. However, because of its emotive component, exercise is likely to have a larger effect, and to date the great majority of our knowledge on this subject comes from exercise studies. In this position statement, a panel of world-leading experts provides a consensus of current knowledge, briefly covering the background, explaining what we think we know with some degree of certainty, exploring continued controversies, and pointing to likely directions for future research. Part one of this position statement focuses on 'immune function and exercise' and part two on 'maintaining immune health'. Part one provides a brief introduction and history (Roy Shephard) followed by sections on: respiratory infections and exercise (Maree Gleeson); cellular innate immune function and exercise (Jeffrey Woods); acquired immunity and exercise (Nicolette Bishop); mucosal immunity and exercise (Michael Gleeson and Nicolette Bishop); immunological methods in exercise immunology (Monika Fleshner); anti-inflammatory effects of physical activity (Charlotte Green and Bente Pedersen); exercise and cancer (Laurie Hoffman-Goetz and Connie Rogers) and finally, "omics" in exercise (Hinnak Northoff, Asghar Abbasi and Perikles Simon). The focus on respiratory infections in exercise has been stimulated by the commonly held beliefs that the frequency of upper respiratory tract infections (URTI) is increased in elite endurance athletes after single bouts of ultra-endurance exercise and during periods of intensive training. The evidence to support these concepts is inconclusive, but supports the idea that exercised-induced immune suppression increases susceptibility to symptoms of infection, particularly around the time of competition, and that upper respiratory symptoms are associated with performance decrements. Conclusions from the debate on whether sore throats are actually caused by infections or are a reflection of other inflammatory stimuli associated with exercise remains unclear. It is widely accepted that acute and chronic exercise alter the number and function of circulating cells of the innate immune system (e.g. neutrophils, monocytes and natural killer (NK) cells). A limited number of animal studies has helped us determine the extent to which these changes alter susceptibility to herpes simplex and influenza virus infection. Unfortunately, we have only 'scratched the surface' regarding whether exercise-induced changes in innate immune function alter infectious disease susceptibility or outcome and whether the purported anti-inflammatory effect of regular exercise is mediated through exercise-induced effects on innate immune cells. We need to know whether exercise alters migration of innate cells and whether this alters disease susceptibility. Although studies in humans have shed light on monocytes, these cells are relatively immature and may not reflect the effects of exercise on fully differentiated tissue macrophages. Currently, there is very little information on the effects of exercise on dendritic cells, which is unfortunate given the powerful influence of these cells in the initiation of immune responses. It is agreed that a lymphocytosis is observed during and immediately after exercise, proportional to exercise intensity and duration, with numbers of cells (T cells and to a lesser extent B cells) falling below pre-exercise levels during the early stages of recovery, before returning to resting values normally within 24 h. Mobilization of T and B cell subsets in this way is largely influenced by the actions of catecholamines. Evidence indicates that acute exercise stimulates T cell subset activation in vivo and in response to mitogen- and antigen-stimulation. Although numerous studies report decreased mitogen- and antigen-stimulated T cell proliferation following acute exercise, the interpretation of these findings may be confounded by alterations in the relative proportion of cells (e.g. T, B and NK cells) in the circulation that can respond to stimulation. Longitudinal training studies in previously sedentary people have failed to show marked changes in T and B cell functions provided that blood samples were taken at least 24 h after the last exercise bout. In contrast, T and B cell functions appear to be sensitive to increases in training load in well-trained athletes, with decreases in circulating numbers of Type 1 T cells, reduced T cell proliferative responses and falls in stimulated B cell Ig synthesis. The cause of this apparent depression in acquired immunity appears to be related to elevated circulating stress hormones, and alterations in the pro/anti-inflammatory cytokine balance in response to exercise. The clinical significance of these changes in acquired immunity with acute exercise and training remains unknown. The production of secretory immunoglobulin A (SIgA) is the major effector function of the mucosal immune system providing the 'first line of defence' against pathogens. To date, the majority of exercise studies have assessed saliva SIgA as a marker of mucosal immunity, but more recently the importance of other antimicrobial proteins in saliva (e.g. alpha-amylase, lactoferrin and lysozyme) has gained greater recognition. Acute bouts of moderate exercise have little impact on mucosal immunity but prolonged exercise and intensified training can evoke decreases in saliva secretion of SIgA. Mechanisms underlying the alterations in mucosal immunity with acute exercise are probably largely related to the activation of the sympathetic nervous system and its associated effects on salivary protein exocytosis and IgA transcytosis. Depressed secretion of SIgA into saliva during periods of intensified training and chronic stress are likely linked to altered activity of the hypothalamic-pituitary-adrenal axis, with inhibitory effects on IgA synthesis and/or transcytosis. Consensus exists that reduced levels of saliva SIgA are associated with increased risk of URTI during heavy training. An important question for exercise immunologists remains: how does one measure immune function in a meaningful way? One approach to assessing immune function that extends beyond blood or salivary measures involves challenging study participants with antigenic stimuli and assessing relevant antigen-driven responses including antigen specific cell-mediated delayed type hypersensitivity responses, or circulating antibody responses. Investigators can inject novel antigens such as keyhole limpet haemocyanin (KLH) to assess development of a primary antibody response (albeit only once) or previously seen antigens such as influenza, where the subsequent antibody response reflects a somewhat more variable mixture of primary, secondary and tertiary responses. Using a novel antigen has the advantage that the investigator can identify the effects of exercise stress on the unique cellular events required for a primary response that using a previously seen antigen (e.g. influenza) does not permit. The results of exercise studies using these approaches indicate that an acute bout of intense exercise suppresses antibody production (e.g. anti-KLH Ig) whereas moderate exercise training can restore optimal antibody responses in the face of stressors and ageing. Because immune function is critical to host survival, the system has evolved a large safety net and redundancy such that it is difficult to determine how much immune function must be lost or gained to reveal changes in host disease susceptibility. There are numerous examples where exercise alters measures of immunity by 15-25%. Whether changes of this magnitude are sufficient to alter host defence, disease susceptibility or severity remains debatable. Chronic inflammation is involved in the pathogenesis of insulin resistance, atherosclerosis, neurodegeneration, and tumour growth. Evidence suggests that the prophylactic effect of exercise may, to some extent, be ascribed to the anti-inflammatory effect of regular exercise mediated via a reduction in visceral fat mass and/or by induction of an anti-inflammatory environment with each bout of exercise (e.g. via increases in circulating anti-inflammatory cytokines including interleukin (IL)-1 receptor antagonist and IL-10). To understand the mechanism(s) of the protective, anti-inflammatory effect of exercise fully, we need to focus on the nature of exercise that is most efficient at allieviating the effects of chronic inflammation in disease. The beneficial effects of endurance exercise are well known; however, the antiinflammatory role of strength training exercises are poorly defined. In addition, the independent contribution of an exercise-induced reduction in visceral fat versus other exercise-induced anti-inflammatory mechanisms needs to be understood better. There is consensus that exercise training protects against some types of cancers. Training also enhances aspects of anti-tumour immunity and reduces inflammatory mediators. However, the evidence linking immunological and inflammatory mechanisms, physical activity, and cancer risk reduction remains tentative. (ABSTRACT TRUNCATED)