- Record: found
- Abstract: found
- Article: found
Anti-Yo antibody-positive paraneoplastic cerebellar degeneration in a patient with possible cholangiocarcinoma: A case report and review of the literature
Read this article at
Abstract
BACKGROUND
Paraneoplastic cerebellar degeneration (PCD), which is rare in clinical practice, is closely related to autoimmunity. Cases positive for anti-Yo antibodies (anti-Purkinje cytoplasmic antibody 1) are the main subtype of PCD. PCD is subacute cerebellar degeneration, and while it progresses over weeks to months, its resultant deficits last much longer. Cancer patients with anti-Yo antibody-positive PCD are very rare. Most of them are breast cancer or ovarian cancer patients but also occasionally lung cancer patients.
CASE SUMMARY
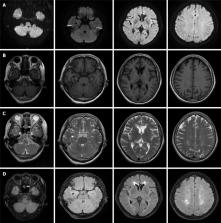
A 61-year-old woman presented with sudden vertigo, nausea, and vomiting for approximately 10 d. The patient's neurological examination showed torsion with downbeat nystagmus and ataxia of the right limb and trunk. Laboratory examination found that the patient's cerebrospinal fluid and serum were anti-Yo antibody-positive, positron emission tomography computed tomography showed an increased metabolic rate in the retroperitoneal lymph nodes, and the pathology of lymph node punctures in the retroperitoneum and neck suggested adenocarcinoma of the pancreaticobiliary duct, which strengthens the hypothesis of paraneoplastic origin. Intravenous immunoglobulin (IVIg) 0.4 g/kg/d for 5 d and methylprednisolone 160 mg for 3 d were initiated, which was reduced to 80 mg for 3 d and then to 40 mg for 7 d. After treatment with IVIg and a steroid, the patient's vertigo and ataxia alleviated.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Recommended diagnostic criteria for paraneoplastic neurological syndromes.
- Record: found
- Abstract: found
- Article: not found
Management of paraneoplastic neurological syndromes: report of an EFNS Task Force.
- Record: found
- Abstract: found
- Article: not found