- Record: found
- Abstract: found
- Article: not found
Does empirical treatment of community-acquired pneumonia with fluoroquinolones delay tuberculosis treatment and result in fluoroquinolone resistance in Mycobacterium tuberculosis? Controversies and solutions
Read this article at
Abstract
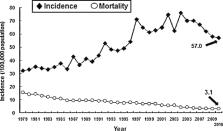
The role of fluoroquinolones (FQs) as empirical therapy for community-acquired pneumonia (CAP) remains controversial in countries with high tuberculosis (TB) endemicity owing to the possibility of delayed TB diagnosis and treatment and the emergence of FQ resistance in Mycobacterium tuberculosis. Although the rates of macrolide-resistant Streptococcus pneumoniae and amoxicillin/clavulanic acid-resistant Haemophilus influenzae have risen to alarming levels, the rates of respiratory FQ (RFQ) resistance amongst these isolates remain relatively low. It is reported that ca. 1–7% of CAP cases are re-diagnosed as pulmonary TB in Asian countries. A longer duration (≥7 days) of symptoms, a history of night sweats, lack of fever (>38 °C), infection involving the upper lobe, presence of cavitary infiltrates, opacity in the lower lung without the presence of air, low total white blood cell count and the presence of lymphopenia are predictive of pulmonary TB. Amongst patients with CAP who reside in TB-endemic countries who are suspected of having TB, imaging studies as well as aggressive microbiological investigations need to be performed early on. Previous exposure to a FQ for >10 days in patients with TB is associated with the emergence of FQ-resistant M. tuberculosis isolates. However, rates of M. tuberculosis isolates with FQ resistance are significantly higher amongst multidrug-resistant M. tuberculosis isolates than amongst susceptible isolates. Consequently, in Taiwan and also in other countries with TB endemicity, a short-course (5-day) regimen of a RFQ is still recommended for empirical therapy for CAP patients if the patient is at low risk for TB.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
Fluoroquinolones are associated with delayed treatment and resistance in tuberculosis: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found
Etiology of community acquired pneumonia among adult patients requiring hospitalization in Taiwan.
- Record: found
- Abstract: found
- Article: not found
