- Record: found
- Abstract: found
- Article: found
Disseminated Juvenile Xanthogranuloma and Hemophagocytic Lymphohistiocytosis Developed During Treatment of Acute Lymphoblastic Leukemia: Case Report
Read this article at
Abstract
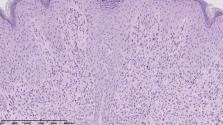
The association between acute lymphoblastic leukemia (ALL), non-Langerhans cell histiocytosis (non-LCH), and hemophagocytic lymphohistiocytosis (HLH), to the best of our knowledge, has not been published to date. Juvenile xanthogranuloma (JXG), as a type of non-LCH, is usually a benign disease limited to the skin. Systemic involvement is rarely reported. The present case report describes a 15-year-old boy diagnosed with disseminated JXG involving skin and bone marrow concurrent with severe symptoms of HLH during ALL therapy. Examination of immunoglobulin heavy chain genes in B-cell precursor leukemic blasts and histiocytes in the skin and bone marrow revealed identical rearrangements, confirming clonal relationship between both diseases. Implementation of corticosteroids, vinblastine, etoposide, cyclosporine, and tocilizumab resulted in partial skin lesion resolution with no improvement of bone marrow function; therefore, hematopoietic stem cell transplantation (HSCT) was eventually performed. The patient's hematological and general status has improved gradually; however, remarkable recovery of skin lesions was observed after empirical antitubercular therapy. Mycobacterium spp. infection should be considered as a possible secondary HLH trigger. Triple association of ALL, non-LCH, and HLH highlights heterogeneity of histiocytic disorders and possible common origin of dendritic and lymphoid cells.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Severe imbalance of IL-18/IL-18BP in patients with secondary hemophagocytic syndrome.
- Record: found
- Abstract: found
- Article: not found
Understanding organ dysfunction in hemophagocytic lymphohistiocytosis.
- Record: found
- Abstract: found
- Article: found