- Record: found
- Abstract: found
- Article: found
An Evaluation of the Effectiveness of the Modalities Used to Deliver Electronic Health Interventions for Chronic Pain: Systematic Review With Network Meta-Analysis
Abstract
Background
Electronic health (eHealth) is the use of information and communication technology in the context of health care and health research. Recently, there has been a rise in the number of eHealth modalities and the frequency with which they are used to deliver technology-assisted self-management interventions for people living with chronic pain. However, there has been little or no research directly comparing these eHealth modalities.
Objective
The aim of this systematic review with a network meta-analysis (NMA) is to compare the effectiveness of eHealth modalities in the context of chronic pain.
Methods
Randomized controlled trials (N>20 per arm) that investigated interventions for adults with chronic pain, delivered via an eHealth modality, were included. Included studies were categorized into their primary node of delivery.
Data were extracted on the primary outcome, pain interference, and secondary outcomes, pain severity, psychological distress, and health-related quality of life. Pairwise meta-analyses were undertaken where possible, and an NMA was conducted to generate indirect comparisons and rankings of modalities for reducing pain interference.
Results
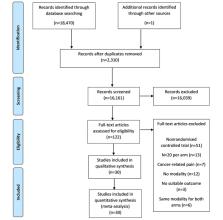
The search returned 18,470 studies with 18,349 being excluded (duplicates=2310; title and abstract=16,039). Of the remaining papers, 30 studies with 5394 randomized participants were included in the review. Rankings tentatively indicated that modern eHealth modalities are the most effective, with a 43% chance that mobile apps delivered the most effective interventions, followed by a 34% chance that interventions delivered via virtual reality were the most effective.
Conclusions
This systematic review with an NMA generated comparisons between eHealth modalities previously not compared to determine which delivered the most effective interventions for the reduction of pain interference in chronic pain patients. There are limitations with this review, in particular, the underrepresented nature of some eHealth modalities included in the analysis. However, in the event that the review is regularly updated, a clear ranking of eHealth modalities for the reduction of pain interference will emerge.
Related collections
Most cited references57

- Record: found
- Abstract: found
- Article: found
Evidence Synthesis for Decision Making 4
- Record: found
- Abstract: found
- Article: not found