- Record: found
- Abstract: found
- Article: not found
Equipment review: Continuous assessment of arterial blood gases
review-article
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Introduction
Determination of arterial oxygenation, arterial CO2 partial pressure and pH is traditionally
performed by intermittent arterial blood sampling. However, this method presents a
number of disadvantages such as the need for iterative and uncomfortable arterial
punctures, and can be associated with substantial blood loss [1,2]. Despite these
major impediments to serial measurements, arterial blood gas values are the most frequently
ordered laboratory examinations in the intensive care unit (ICU) and the operating
room [3]. In the ICU, except for once-daily analysis which represents a `spot check'
of the physiological state of the patient, indications for sampling are essentially
the result of a deleterious event [4]. In these situations, sampling depends greatly
upon the judgement of the physician, nurse or other health care provider to determine
whether a blood gas measurement is needed. The delay between the event itself and
blood sampling, plus the delay in obtaining the results, means that this sort of analysis
may be misleading. For example, clinically important changes in a patient's blood
gas status may go undetected or may occur after a sample has been drawn and while
it is being analysed [5]. Moreover, considerable spontaneous variation in blood gases
frequently occurs, even in stable ICU patients [6].
Because clinical decisions need to be made on the basis of trends in blood gases as
well as with the rapid detection of an acute event [6,7], continuous non-invasive
monitoring techniques, such as pulse-oximetry and continuous capnography, have been
developed. Unfortunately, these devices are not always accurate or reliable in acute
situations such as shock, hypothermia, or during the use of vasopressors [8,9]. Moreover,
pulse-oximetry does not measure oxygen tension, and major drawbacks also exist for
continuous capnography.
Continuous arterial blood gas monitoring systems?
Since the 1980's several attempts has been made to develop equipment which is able
to overcome the disadvantages of intermittent arterial blood sampling and those of
non-invasive monitoring. The goal of the research has been to develop a real-time
continuous blood gas monitoring system.
This led to the development of `blood gas monitors' which were defined as `patient-dedicated
apparatus used to measure arterial pH, PaCO2 and PaO2 without permanently removing
blood samples' [10,11]. Two different techniques of blood gas measurement, based on
electro-chemical or optical principles, were initially proposed [12]. However, blood
gas electrodes were not readily adaptable for this type of monitoring because they
required frequent replenishment of reagents and recalibration.
Later, new technology was developed that monitored blood gas levels using optical
sensors (optodes). A uv light source is pulsed, at a predetermined frequency, at specific
dyes in the blood stream which are sensitive to one or other analyte. The light is
re-emitted at a lower intensity and the decrease in fluorescence is proportional to
the concentration of analyte in the dye [13,14]. The monitor provides the computer
support needed to calculate the blood gas values using the signal from the sensing
element. Two different apparatus, which differ in the location of the sensing element,
were developed: extra-arterial blood gas (EABG) monitors and intra-arterial blood
gas (IABG) monitors.
Extra-arterial blood gas monitors
The EABG system utilizes optodes which are externally attached to the arterial catheter
(CDI 2000 Blood Gas Monitoring System: CDI-3M Healthcare, Tustin, CA), in an attempt
to avoid the patient interface problems observed with the first IABG devices [15,16].
This on demand catheter allows direct blood gas analysis at the bedside [5,6,7,8,15]
and significantly reduces the delay in obtaining results. Moreover, different studies
have demonstrated accuracy and precision comparable with conventional blood gas analysers,
even with blood abnormalities in acutely ill patients [1,17,18,19]. This system seems
to demonstrate greater precision for PaO2 analysis than continuous IABG monitors [20].
However, the on-demand monitoring system is not continuous. Whenever a blood gas value
is required, blood is drawn up into the arterial line tubing past a cassette containing
optodes measuring pH, PaCO2 and PaO2. The rate of measurements taken is obviously
dependent on the frequency of the decision to draw a sample [21]. Such monitors do
not obviate the problems associated with dependence on clinical judgement as to when
samples should be drawn. Moreover, trends are not recorded and accurate detection
of life-threatening events associated with acute changes in blood gases is not achieved.
This technique does not, therefore, strictly adhere to the definition of continuous
assessment of arterial blood gases [21].
Intra-arterial blood gas monitors
Unlike on-demand catheters, IABG monitors offer the interesting possibility of ensuring
real-time continuous measurement of arterial blood gases [22]. Based on the same optode
technology as the EABG devices, this technique differs because the sensor is directly
inserted into the arterial blood stream. Unfortunately, until recently none of these
devices had demonstrated adequate clinical performance, [15,16,23,24,25,26]. Their
consistency and reliability were unacceptable because of significant malfunctions
and inconsistencies that were shown to be attributable to the intra-arterial environment
[15]. Aberrant blood gas values, obtained particularly in cases of hypotension or
vascular construction were attributed to the `wall-stress effect' on the sensing element
[15,16].
Since the first attempts, however, several companies have further developed optode-based
IABG monitors: the PB 3300 IABG Monitor (Puritan-Bennett Corporation, Los Angeles,
CA), the Paratrend 7 Intravascular Blood Gas Monitoring System (Biomedical Sensors
Ltd, Malvern, PA), and the Optex BioSentry Optode System (Optex Bio-medical Inc, The
Woodlands, TX). These continuous monitoring systems consist of a sterile, disposable,
fiber optic sensor introduced through a 20 gauge arterial catheter, and a microprocessor-controlled
monitor with a self-contained calibration unit and detachable display and control
panel. The sensor contains small optical fibers (one fiber for each analyte) which
are bundled together in a biocompatible package. Each fiber is about he diameter of
a human hair. Even bundled, the entire sensor is small enough to be inserted through
a 20 gauge catheter (1 mm). After in vitro calibration in a sterile cuvette filled
with a buffer solution, the sensor is inserted via an arterial catheter into the patient's
arterial blood stream. No further calibration is needed. A Y-port built into the sensor
permits continuous blood pressure monitoring and allows blood withdrawal. The sensing
element is at the tip of the optic fibers. An optical signal is processed by the monitor
and displayed as the patient's values every 20 s, without external intervention, and
the display screen provides current numerical values and real-time trends for each
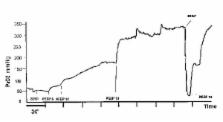
parameter, allowing continuous monitoring. An example of a real-time trend of PaO2
during a PEEP trial is shown in Fig 1.
The main advantage of continuous monitoring is having reliable values of blood gases
available on-line, especially in life-threatening situations. Moreover, IABG monitors
could potentially benefit respiratory care in the ICU, particularly in patients with
unstable respiratory status, and might replace standard systems of blood gas sampling.
However, it has to be demonstrated that the equipment is accurate, precise and reliable
for wide ranging and unstable blood gas levels, characteristic of acutely ill patients
entering an ICU.
Larson et al [27] have evaluated one of these new continuous IABG monitoring systems
(PB 3300, Puritan-Bennett Corporation, Los Angeles, CA) in patients undergoing surgical
procedures and postoperative intensive care. The accuracy of this particular continuous
IABG monitor was found to be acceptable when compared to conventional arterial blood
samples for values observed during and after uncomplicated operative procedures. Arterial
blood gas and pH values, however, were for the most part within normal physiological
ranges. Two further studies [28,29] in the ICU have confirmed these results. Haller
et al [29] evaluated the performance of this device in critically ill patients with
respiratory failure. They also found a high precision for PaO2, PaCO2 and pH. However,
only a small fraction of their 487 pairs of data were in the range of extremely abnormal
blood gas values. The same results were demonstrated, in similar conditions, with
the Paratrend 7 Intravascular Blood Gas Monitoring System [30,31]. However, in their
report, Venkatesh et al [31] withdrew one patient (Pt 8) from their analysis because
he demonstrated a large bias and a considerably higher precision than the rest of
the patients (n = 13), especially in the PaO2 comparison.
All of these studies, however, concluded that an acceptable level of clinical accuracy
was found, even for PaO2 and demonstrated an improvement in the performance of the
new IABG monitors when compared with previously published data [27,28,29,31]. In fact,
Venkatesh et al enthusiastically claimed that the sensor will become `an important
tool in the management of critically ill patient [31]. However, this very optimistic
view is not complete' justified.
In a recent study, we reasoned that the clinical performance of continuous IABG monitors
should be tested in extreme situations such as `abnormal' ranges of PaO2, PaCO2 and
pH, and during episodes of hemodynamic instability where non-invasive monitoring failed.
These tests were done to discover whether these devices were able to provide accurate
information in critically ill patients [20]. Our results indicated that, compared
to classical electrochemical measurement of arterial blood samples, continuous IABG
monitoring essentially provided reliable and clinically accurate blood gas results
for pH and PaCO2 even with highly abnormal values (PaCO2 > 90 mmHg, pH < 7.1). Furthermore,
when looking at sequential changes, continuous IABG monitoring and arterial blood
sampling were very similar indicating that continuous IABG is able to follow variations
in blood gases successfully over time. This new continuous monitoring system was also
reliable and accurate during episodes of low blood pressure even when pulse-oximetry
failed. However, although we found the same good results for PaCO2 and pH, our findings
differed for PaO2. Whatever the test conditions, the differences between the electrochemical
and fluorescent optode (IABG) technologies appeared greater, and unacceptable, for
PaO2. Differences as high as 30 mmHg were found [20]. Although there are inherent
errors in both methods of measurement, pre-analytic and analytic errors in conventional
blood gas analysis prevent this method from being regarded as `the gold standard'
to which IABG monitoring is compared [27]. However, the fact remains that the large
interindividual difference in the performance of continuous IABG catheters observed
for PaO2 suggests that at least the PaO2 analyzer was not accurate enough [20].
Apart from the discrepancy for PaO2, the other important problem observed was the
brittleness of the fibers. Six of the 21 fibers were broken as soon as they were inserted.
A simple flexion of the hand was enough to break the device [20].
As shown by our experience, the sensor is fragile and easily damaged during insertion,
particularly the oxygen component which is at the tip of the sensor. To be clinically
useful the sensor must be rugged or sheathed in a way that would prevent its damage
at insertion [32]. In addition to the improvement in the accuracy of PaO2 measurements,
this is an important consideration for the future development of such equipment.
Since our own evaluation of the PB 3300, this device has been withdrawn for economic
reasons. At present, the only manufacturer of continuous IABG monitoring equipment
is Pfizer Biomedical Sensors, with their Paratrend 7. This device has achieved the
same results as the PB 3300, but is also affected by the same limitations that we
have noted for the PB 3300 [31,33].
Conclusion
Despite these words of caution, especially concerning the quality of the PaO2 analyser
and the brittleness of the fibers, there will hopefully be chances to improve this
new technology, and we believe that continuous IABG analysis should have many applications
in the future. However, even after these technical problems are resolved, two questions
still remain:
1. Does this technology really improve patient care?
2. What is the cost-benefit ratio of such an expensive device?
Although some authors have suggested that the development of such systems would have
important implications for critical care practice and cost efficiency [34,35], no
trial has yet focused on these fundamental questions. Until such studies are completed
and evaluated, it is reasonable to agree with Dr C Larson, that `continuous arterial
blood gas monitoring is a technology in transition whose fate is yet unknown'[32].
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements.
M S Kruskall, B Smoller (1986)
- Record: found
- Abstract: found
- Article: not found
Accuracy of response of six pulse oximeters to profound hypoxia.
K Naifeh, J W Severinghaus (1987)
- Record: found
- Abstract: found
- Article: not found
Variability of arterial blood gas values in stable patients in the ICU.
Nicholas Marini, Kenneth D Pierson, S. Thorson … (1983)
