- Record: found
- Abstract: found
- Article: found
Attention-deficit hyperactivity disorder in children born to mothers with infertility: a population-based cohort study
Read this article at
Abstract
STUDY QUESTION
Is the risk of attention-deficit hyperactivity disorder (ADHD) increased in children born to mothers with infertility, or after receipt of fertility treatment, compared to mothers with unassisted conception?
SUMMARY ANSWER
Infertility itself may be associated with ADHD in the offspring, which is not amplified by the use of fertility treatment.
WHAT IS KNOWN ALREADY
Infertility, and use of fertility treatment, is common. The long-term neurodevelopmental outcome of a child born to a mother with infertility, including the risk of ADHD, remains unclear.
STUDY DESIGN, SIZE, DURATION
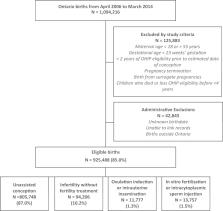
This population-based cohort study comprised all singleton and multiple hospital births in Ontario, Canada, 2006–2014. Outcomes were assessed up to June 2020.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Linked administrative datasets were used to capture all hospital births in Ontario, maternal health and pregnancy measures, fertility treatment and child outcomes. Included were all children born at ≥24 weeks gestation between 2006 and 2014, and who were alive at age 4 years. The main exposure was mode of conception, namely (i) unassisted conception (reference group), (ii) infertility without fertility treatment (history of an infertility consultation with a physician within 2 years prior to conception but no fertility treatment), (iii) ovulation induction (OI) or intrauterine insemination (IUI) and (iv) IVF or intracytoplasmic sperm injection (ICSI). The main outcome was a diagnosis of ADHD after age 4 years and assessed up to June 2020. Hazard ratios (HRs) were adjusted for maternal age, income quintile, rurality, immigration status, smoking, obesity, parity, any drug or alcohol use, maternal history of mental illness including ADHD, pre-pregnancy diabetes mellitus or chronic hypertension and infant sex. In addition, we performed pre-planned stratified analyses by mode of delivery (vaginal or caesarean delivery), infant sex, multiplicity (singleton or multiple), timing of birth (term or preterm <37 weeks) and neonatal adverse morbidity (absent or present).
MAIN RESULTS AND THE ROLE OF CHANCE
The study included 925 488 children born to 663 144 mothers, of whom 805 748 (87%) were from an unassisted conception, 94 206 (10.2%) followed infertility but no fertility treatment, 11 777 (1.3%) followed OI/IUI and 13 757 (1.5%) followed IVF/ICSI. Starting at age 4 years, children were followed for a median (interquartile range) of 6 (4–8) years. ADHD occurred among 7.0% of offspring in the unassisted conception group, 7.5% in the infertility without fertility treatment group, 6.8% in the OI/IUI group and 6.3% in the IVF/ICSI group. The incidence rate (per 1000 person-years) of ADHD was 12.0 among children in the unassisted conception group, 12.8 in the infertility without fertility treatment group, 12.9 in the OI/IUI group and 12.2 in the IVF/ICSI group. Relative to the unassisted conception group, the adjusted HR for ADHD was 1.19 (95% CI 1.16–1.22) in the infertility without fertility treatment group, 1.09 (95% CI 1.01–1.17) in the OI/IUI group and 1.12 (95% CI 1.04–1.20) in the IVF/ICSI group. In the stratified analyses, these patterns of risk for ADHD were largely preserved. An exception was seen in the sex-stratified analyses, wherein females had lower absolute rates of ADHD but relatively higher HRs compared with that seen among males.
LIMITATIONS, REASONS FOR CAUTION
Some mothers in the isolated infertility group may have received undocumented OI oral therapy, thereby leading to possible misclassification of their exposure status. Parenting behaviour, schooling and paternal mental health measures were not known, leading to potential residual confounding.
WIDER IMPLICATIONS OF THE FINDINGS
Infertility, even without treatment, is a modest risk factor for the development of ADHD in childhood. The reason underlying this finding warrants further study.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Prenatal Risk Factors and the Etiology of ADHD—Review of Existing Evidence
- Record: found
- Abstract: found
- Article: not found
A comprehensive assessment of parental age and psychiatric disorders.
- Record: found
- Abstract: found
- Article: not found