- Record: found
- Abstract: found
- Article: found
Comparison of Outcomes After Transcatheter Aortic Valve Replacement vs Surgical Aortic Valve Replacement Among Patients With Aortic Stenosis at Low Operative Risk
Read this article at
Abstract
This comparative effectiveness cohort study examines 30-day and 3-year survival among Finnish patients with aortic stenosis at low operative risk who underwent transcatheter aortic valve replacement compared with surgical aortic valve replacement.
Key Points
Question
Does transcatheter aortic valve replacement achieve similar results compared with surgical aortic valve replacement in patients at low operative risk with severe aortic stenosis?
Abstract
Importance
Transcatheter aortic valve replacement (TAVR) has been shown to be a valid alternative to surgical aortic valve replacement (SAVR) in patients at high operative risk with severe aortic stenosis (AS). However, the evidence of the benefits and harms of TAVR in patients at low operative risk is still scarce.
Objective
To compare the short-term and midterm outcomes after TAVR and SAVR in low-risk patients with AS.
Design, Setting, and Participants
This retrospective comparative effectiveness cohort study used data from the Nationwide Finnish Registry of Transcatheter and Surgical Aortic Valve Replacement for Aortic Valve Stenosis of patients at low operative risk who underwent TAVR or SAVR with a bioprosthesis for severe AS from January 1, 2008, to November 30, 2017. Low operative risk was defined as a Society of Thoracic Surgeons Predicted Risk of Mortality score less than 3% without other comorbidities of clinical relevance. One-to-one propensity score matching was performed to adjust for baseline covariates between the TAVR and SAVR cohorts.
Exposures
Primary TAVR or SAVR with a bioprosthesis for AS with or without associated coronary revascularization.
Results
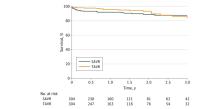
Overall, 2841 patients (mean [SD] age, 74.0 [6.2] years; 1560 [54.9%] men) fulfilled the inclusion criteria and were included in the analysis; TAVR was performed in 325 patients and SAVR in 2516 patients. Propensity score matching produced 304 pairs with similar baseline characteristics. Third-generation devices were used in 263 patients (86.5%) who underwent TAVR. Among these matched pairs, 30-day mortality was 1.3% after TAVR and 3.6% after SAVR ( P = .12). Three-year survival was similar in the study cohorts (TAVR, 85.7%; SAVR, 87.7%; P = .45). Interaction tests found no differences in terms of 3-year survival between the study cohorts in patients younger than vs older than 80 years or in patients who received recent aortic valve prostheses vs those who did not.
Conclusions and Relevance
Transcatheter aortic valve replacement using mostly third-generation devices achieved similar short- and mid-term survival compared with SAVR in low-risk patients. Further studies are needed to assess the long-term durability of TAVR prostheses before extending their use to low-risk patients.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Transcatheter Versus Surgical Aortic Valve Replacement in Patients With Severe Aortic Valve Stenosis
- Record: found
- Abstract: not found
- Article: not found
Durability of Transcatheter and Surgical Bioprosthetic Aortic Valves in Patients at Lower Surgical Risk
- Record: found
- Abstract: found
- Article: not found