- Record: found
- Abstract: found
- Article: found
Leukoaraiosis Is Not Associated With Recovery From Aphasia in the First Year After Stroke
Read this article at
Abstract
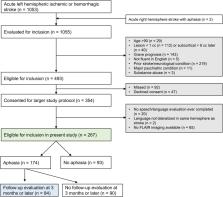
After a stroke, individuals with aphasia often recover to a certain extent over time. This recovery process may be dependent on the health of surviving brain regions. Leukoaraiosis (white matter hyperintensities on MRI reflecting cerebral small vessel disease) is one indication of compromised brain health and is associated with cognitive and motor impairment. Previous studies have suggested that leukoaraiosis may be a clinically relevant predictor of aphasia outcomes and recovery, although findings have been inconsistent. We investigated the relationship between leukoaraiosis and aphasia in the first year after stroke. We recruited 267 patients with acute left hemispheric stroke and coincident fluid attenuated inversion recovery MRI. Patients were evaluated for aphasia within 5 days of stroke, and 174 patients presented with aphasia acutely. Of these, 84 patients were evaluated at ∼3 months post-stroke or later to assess longer-term speech and language outcomes. Multivariable regression models were fit to the data to identify any relationships between leukoaraiosis and initial aphasia severity, extent of recovery, or longer-term aphasia severity. We found that leukoaraiosis was present to varying degrees in 90% of patients. However, leukoaraiosis did not predict initial aphasia severity, aphasia recovery, or longer-term aphasia severity. The lack of any relationship between leukoaraiosis severity and aphasia recovery may reflect the anatomical distribution of cerebral small vessel disease, which is largely medial to the white matter pathways that are critical for speech and language function.
Related collections
Most cited references42
- Record: found
- Abstract: not found
- Article: not found
Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology.
- Record: found
- Abstract: found
- Article: not found
MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging.
- Record: found
- Abstract: found
- Article: not found