- Record: found
- Abstract: found
- Article: found
Cost of hemodialysis in a public sector tertiary hospital of India
Read this article at
ABSTRACT
Introduction
Nearly 220000 patients are diagnosed with end-stage renal disease (ESRD) every year, which calls for an additional demand of 34 million dialysis sessions in India. The government of India has announced a National Dialysis Programme to provide for free dialysis in public hospitals. In this article we estimate the overall cost of performing hemodialysis (HD) in a tertiary care hospital. Second, we assess the catastrophic impact of out-of-pocket expenditures (OOPEs) for HD on households and its determinants.
Methods
The economic health system cost of HD was estimated using bottom-up costing methods. All resources, capital and recurrent, utilized for service delivery from April 2015 to March 2016 were identified, measured and valued. Capital costs were annualized after accounting for their useful life and discounting at 3% for future years. Sensitivity analyses were undertaken to determine the effect of variation in the input prices and other assumptions on the annual health system cost. OOPEs were assessed by interviewing 108 patients undergoing HD in the study hospital to account for costs from the patient’s perspective. The prevalence of catastrophic health expenditures (CHEs) was computed per threshold of 40% of non-food expenditures.
Results
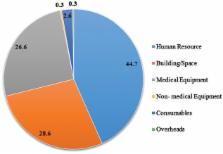
The overall average cost incurred by the health system per HD session was INR 4148 (US$64). Adjusting for capacity utilization, the health system incurred INR 3025 (US$47) per HD at 100% bed occupancy. The mean OOPE per patient per session was INR 2838 (US$44; 95% confidence interval US$34–55). The major components of this OOPE were medicines and consumables (64.1%). The prevalence of a CHE per HD session was 11.1%.
Related collections
Most cited references29

- Record: found
- Abstract: found
- Article: found
Impact of Publicly Financed Health Insurance Schemes on Healthcare Utilization and Financial Risk Protection in India: A Systematic Review
- Record: found
- Abstract: found
- Article: not found
The cost of epilepsy in the United States: an estimate from population-based clinical and survey data.
- Record: found
- Abstract: found
- Article: not found