- Record: found
- Abstract: found
- Article: found
Randomized Trial of Compression Duration After Transradial Cardiac Catheterization and Intervention
Read this article at
Abstract
Background
Radial artery occlusion is a known complication following transradial cardiac catheterization. A shorter duration of postprocedural radial clamp time may reduce radial artery occlusion ( RAO) but might be associated with incomplete hemostasis.
Methods and Results
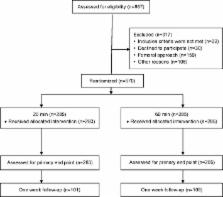
In total, 568 patients undergoing transradial diagnostic cardiac catheterization were randomly assigned to either 20 minutes (ultrashort) or 60 minutes (short) hemostatic compression time using patent hemostasis. Subsequently, clamp pressure was reduced gradually over 20 minutes. Access site hemostasis and RAO were assessed after clamp removal. Repeated assessment of RAO was determined at 1 week in 210 (37%) patients. Mean age was 64±11 years, and 30% were female. Percutaneous coronary intervention was performed in 161 patients. RAO immediately after clamp removal was documented in 14 (4.9%) and 8 (2.8%) patients in the 20‐ and 60‐minute clamp application groups, respectively ( P=0.19). The incidence of grade 1 hematoma was higher in the 20‐minute group (6.7% versus 2.5%, P=0.015). RAO at 1 week after the procedure was 2.9% and 0.9% in the 20‐ and 60‐minute groups, respectively ( P=0.36). Requirement for clamp retightening (36% versus 16%, P=0.01) was higher among patients who had RAO. Need for clamp retightening was the only independent predictor of RAO ( P=0.04).
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials.
- Record: found
- Abstract: found
- Article: not found