- Record: found
- Abstract: found
- Article: found
Tracheostomy in critically ill patients with SARS 2 COVID-19 infection: a prospective observational multi-center study of short- and long-term outcomes
Abstract
Background
We report the characteristics, timing, and factors related to the decision to perform a tracheostomy in patients with confirmed COVID-19 infection admitted to eight Italian intensive care units (ICUs).
Materials and methods
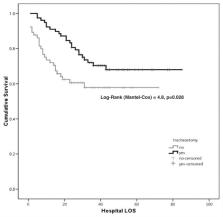
Prospective observational cohort study of patients with COVID-19 disease on mechanical ventilation. Long-term functional impairment (up to 180 days’ post-hospital discharge) was assessed using the Karnofsky scale. Kaplan–Meier analysis assessed differences in survival and freedom from tracheostomy in relation to ICU stay. Cox regression model was used to assess which variables impacted on tracheostomy as a categorical outcome.
Results
A total of 248 patients were recruited in the eight participating ICUs. Patients undergoing tracheostomy ( n = 128) had longer ICU (25 (18–36) vs. 10 (7–16), P = 0.001) and hospital (37 (26.5–50) vs. 19 (8.5–34.5) P = 0.02) stays. ICU and hospital mortality of patients tracheostomized was 34% and 37%, respectively. Cumulative survival Kaplan–Meier analysis documented improved survival rates in patients undergoing tracheostomy (Log-Rank, Mantel–Cox = 4.8, P = 0.028). Median Karnofsky scale values improved over time but were similar between survivors receiving or not receiving tracheostomy. No healthcare worker involved in the tracheostomy procedure developed COVID-19 infection during the study period.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
A Novel Coronavirus from Patients with Pneumonia in China, 2019
- Record: found
- Abstract: found
- Article: not found
