- Record: found
- Abstract: found
- Article: found
Validation of the HIV Pre-exposure Prophylaxis Stigma Scale: Performance of Likert and Semantic Differential Scale Versions
Read this article at
Abstract
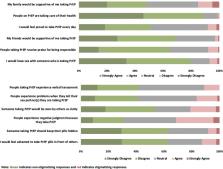
Stigma regarding HIV pre-exposure prophylaxis (PrEP) is commonly implicated as a factor limiting the scale-up of this highly effective HIV prevention modality. To quantify and characterize PrEP stigma, we developed and validated a brief HIV PrEP Stigma Scale (HPSS) among a group of 279 men who have sex with men (MSM). Scale development was informed by a theoretical model to enhance content validity. We assessed two scale versions, Semantic Differential and Likert, randomizing the order in which scales were presented to participants. Both scales demonstrated high internal consistency. The Likert scale had substantially better construct validity and was selected as the preferred option. Scale scores demonstrated construct validity through association with constructs of interest: healthcare distrust, HIV knowledge, perceived proportion of friends/partners on PrEP, perceived community evaluation of PrEP, and perceived effectiveness of PrEP. The scale accounted for 25% of the total variance in reported willingness to be on PrEP, indicating the substantial role PrEP stigma may have on decisions to initiate PrEP. Given increased efforts to roll-out PrEP, having a valid tool to determine the level and types of PrEP stigma in individuals, groups, and communities can help direct implementation plans, identify goals for stigma reduction, and monitor progress over time.
Resumen
El estigma relacionado con la profilaxis pre-exposición para la prevención del VIH (PrEP, por sus siglas en inglés) ha sido identificado como un factor que limita la implementación a gran escala de esta efectiva modalidad de prevención del VIH. Para poder cuantificar y caracterizar el estigma relacionado al PrEP, desarrollamos y validamos una breve Escala de Estigma al PrEP (HPSS, por sus siglas en inglés) con un grupo de 279 hombres que tienen sexo con hombres. El desarrollo de la escala se basó en un modelo teórico para optimizar la validez de contenido. Evaluamos dos versiones de la escala, Diferencial Semántico y Likert, alternando aleatoriamente el orden en que se presentaron las escalas a los participantes. Ambas escalas demostraron alta consistencia interna. La escala Likert tuvo una mejor validez de constructo y fue seleccionada como la opción preferencial. Los puntajes de la escala demostraron validez de constructo a través de su asociación con las siguientes construcciones de interés: desconfianza en el sistema de salud, conocimiento acerca del VIH, percepción de la proporción de amigos/compañeros que toman PrEP, percepción de la evaluación comunitaria acerca del PrEP, y percepción de la efectividad del PrEP. La escala representó el 25% de la varianza total de la disposición a tomar PrEP, lo que indica el importante rol que el estigma asociado al PrEP puede tener en la decisión de empezar a tomar PrEP. Dado el aumento de los esfuerzos para implementar PrEP, el contar con una herramienta válida para determinar el nivel y los tipos de estigma relacionado al PrEP en individuos, grupos y comunidades puede ayudar a dar dirección a los planes de implementación, a identificar objetivos para la reducción del estigma y a monitorear el progreso a lo largo del tiempo.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures.
- Record: found
- Abstract: found
- Article: not found
From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City.
- Record: found
- Abstract: found
- Article: not found