- Record: found
- Abstract: found
- Article: found
Impacts of Nontuberculous Mycobacteria Isolates in Non-cystic Fibrosis Bronchiectasis: A 16-Year Cohort Study in Taiwan
Read this article at
Abstract
Background
The prevalence of nontuberculous mycobacteria (NTM) in patients with chronic respiratory disease has increased. The implication of NTM in non- CF bronchiectasis remained controversial. This study investigated the impact of NTM in non- CF bronchiectasis in Taiwan.
Methods
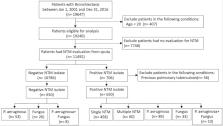
Clinical manifestation, imaging, and microbiological data were retrieved from the Chang Gung Research Database, the largest electronic medical record-based database in Taiwan. Patients with bronchiectasis during 2001–2016 were included. Cox proportional hazard model was employed to compare outcomes between patients with negative and positive NTM isolates after 1:1 propensity score matching.
Results
A total of 19,647 non- CF bronchiectasis patients were enrolled and 11,492 patients were eligible for analysis after exclusion screening. Finally, patients with negative and positive NTM isolates—650 each—were analyzed after propensity score matching. The patients with negative NTM isolates were divided into three groups: Pseudomonas aeruginosa isolates ( n = 53); fungus isolates ( n = 26); and concomitant P. aeruginosa and fungus isolates ( n = 8). The patients with positive NTM isolates were divided into five groups: single NTM isolate ( n = 458); multiple NTM isolates ( n = 60); concomitant NTM and P. aeruginosa isolates ( n = 89); concomitant NTM and fungus isolates ( n = 33); and concomitant NTM, P. aeruginosa, and fungus isolates ( n = 10). Patients with P. aeruginosa isolates; concomitant NTM and P. aeruginosa isolates; concomitant NTM, P. aeruginosa, and fungus isolates had independently associated with respiratory failure and death. Patients with single or multiple NTM isolates were not related to ventilator use, but both were independent risk factor for mortality.
Conclusion
NTM, either combined with P. aeruginosa or fungus, exhibited more frequent exacerbations in non- CF bronchiectasis patients. Moreover, NTM predicted mortality in non- CF bronchiectasis patients and were also correlated to respiratory failure while concomitantly isolated with P. aeruginosa and fungus.
Related collections
Most cited references37
- Record: found
- Abstract: not found
- Article: not found
Standardisation of spirometry.
- Record: found
- Abstract: found
- Article: not found
The bronchiectasis severity index. An international derivation and validation study.
- Record: found
- Abstract: found
- Article: not found