- Record: found
- Abstract: found
- Article: found
Leading Comorbidity associated with 30-day post-anesthetic mortality in geriatric surgical patients in Taiwan: a retrospective study from the health insurance data
Read this article at
Abstract
Background
Elderly patients with aged physical status and increased underlying disease suffered from more postoperative complication and mortality. We design this retrospective cohort study to investigate the relationship between existing comorbidity of elder patients and 30 day post-anesthetic mortality by using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) from Health Insurance Database.
Methods
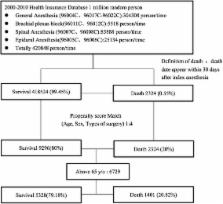
Patients aged above 65 years old who received anesthesia between 2000 and 2010 were included from 1 million Longitudinal Health Insurance Database in (LHID) 2005 in Taiwan. We use age, sex, type of surgery to calculate propensity score and match death group and survival one with 1:4 ratio (death: survival = 1401: 5823). Multivariate logistic model with stepwise variable selection was employed to investigate the factors affecting death 30 days after anesthesia.
Results
Thirty seven comorbidities can independently predict the post-anesthetic mortality. In our study, the leading comorbidities predict post-anesthetic mortality is chronic renal disease (OR = 2.806), acute myocardial infarction (OR = 4.58), and intracranial hemorrhage (OR = 3.758).
Conclusions
In this study, we present the leading comorbidity contributing to the postoperative mortality in elderly patients in Taiwan from National Health Insurance Database. Chronic renal failure is the leading contributing comorbidity of 30 days mortality after anesthesia in Taiwan which can be explained by the great number of hemodialysis and prolong life span under National Taiwan Health Insurance. Large scale database can offer enormous information which can help to improve quality of medical care.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Surgical risk factors, morbidity, and mortality in elderly patients.
- Record: found
- Abstract: found
- Article: not found
ASA class is a reliable independent predictor of medical complications and mortality following surgery.
- Record: found
- Abstract: found
- Article: not found