- Record: found
- Abstract: found
- Article: found
Does fragmented cancer care affect survival? Analysis of gastric cancer patients using national insurance claim data
Read this article at
Abstract
Background
We aimed to investigate the association between fragmented cancer care in the early phase after cancer diagnosis and patient outcomes using national insurance claim data.
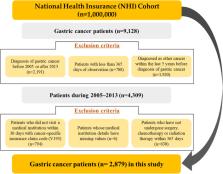
Methods
From a nationwide sampled cohort database, we identified National Health Insurance beneficiaries diagnosed with gastric cancer (ICD-10: C16) in South Korea during 2005–2013. We analyzed the results of a multiple logistic regression analysis using the generalized estimated equation model to investigate which patient and institution characteristics affected fragmented cancer care during the first year after diagnosis. Then, survival analysis using the Cox proportional hazard model was conducted to investigate the association between fragmented cancer care and five-year mortality.
Results
Of 2879 gastric cancer patients, 11.9% received fragmented cancer care by changing their most visited medical institution during the first year after diagnosis. We found that patients with fragmented cancer care had a higher risk of five-year mortality (HR: 1.310, 95% CI: 1.023–1.677). This association was evident among patients who only received chemotherapy or radiotherapy (HR: 1.633, 95% CI: 1.005–2.654).
Conclusions
Fragmented cancer care was associated with increased risk of five-year mortality. Additionally, changes in the most visited medical institution occurred more frequently in either patients with severe conditions or patients who mainly visited smaller medical institutions. Further study is warranted to confirm these findings and examine a causal relationship between fragmented cancer care and survival.
Related collections
Most cited references26
- Record: found
- Abstract: not found
- Article: not found
Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up.
- Record: found
- Abstract: found
- Article: not found
Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer.

- Record: found
- Abstract: found
- Article: found