- Record: found
- Abstract: found
- Article: found
Acetaminophen-Induced Hepatotoxicity: a Comprehensive Update
Read this article at
Abstract
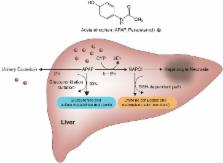
Hepatic injury and subsequent hepatic failure due to both intentional and non-intentional overdose of acetaminophen (APAP) has affected patients for decades, and involves the cornerstone metabolic pathways which take place in the microsomes within hepatocytes. APAP hepatotoxicity remains a global issue; in the United States, in particular, it accounts for more than 50% of overdose-related acute liver failure and approximately 20% of the liver transplant cases. The pathophysiology, disease course and management of acute liver failure secondary to APAP toxicity remain to be precisely elucidated, and adverse patient outcomes with increased morbidity and mortality continue to occur. Although APAP hepatotoxicity follows a predictable timeline of hepatic failure, its clinical presentation might vary. N-acetylcysteine (NAC) therapy is considered as the mainstay therapy, but liver transplantation might represent a life-saving procedure for selected patients. Future research focus in this field may benefit from shifting towards obtaining antidotal knowledge at the molecular level, with focus on the underlying molecular signaling pathways.
Related collections
Most cited references63
- Record: found
- Abstract: found
- Article: not found
Metabolism and disposition of acetaminophen: recent advances in relation to hepatotoxicity and diagnosis.
- Record: found
- Abstract: found
- Article: not found
Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial.
- Record: found
- Abstract: not found
- Article: not found