- Record: found
- Abstract: found
- Article: found
PTH-dependence of the effectiveness of cinacalcet in hemodialysis patients with secondary hyperparathyroidism
Read this article at
Abstract
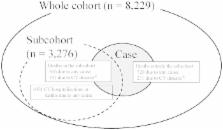
Cinacalcet lowers parathyroid hormone levels. Whether it can prolong survival of people with chronic kidney disease (CKD) complicated by secondary hyperparathyroidism (SHPT) remains controversial, in part because a recent randomized trial excluded patients with iPTH <300 pg/ml. We examined cinacalcet’s effects at different iPTH levels. This was a prospective case-cohort and cohort study involving 8229 patients with CKD stage 5D requiring maintenance hemodialysis who had SHPT. We studied relationships between cinacalcet initiation and important clinical outcomes. To avoid confounding by treatment selection, we used marginal structural models, adjusting for time-dependent confounders. Over a mean of 33 months, cinacalcet was more effective in patients with more severe SHPT. In patients with iPTH ≥500 pg/ml, the reduction in the risk of death from any cause was about 50% (Incidence Rate Ratio [IRR] = 0.49; 95% Confidence Interval [95% CI]: 0.29–0.82). For a composite of cardiovascular hospitalization and mortality, the association was not statistically significant, but the IRR was 0.67 (95% CI: 0.43–1.06). These findings indicate that decisions about using cinacalcet should take into account the severity of SHPT.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men.
- Record: found
- Abstract: found
- Article: not found
Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis.
- Record: found
- Abstract: found
- Article: not found