- Record: found
- Abstract: found
- Article: found
Gitelman’s Syndrome in Pregnancy With Adverse Foetal Outcome: A Case Report
Read this article at
Abstract
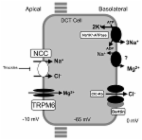
Gitelman’s syndrome (GS) is a disorder characterized by hypokalaemia, hypomagnesemia, hypocalciuric and metabolic alkalosis. Despite the fact that it affects women of child-bearing age, only limited information is available regarding its impact on maternal and foetal outcome. We present the case of an un-booked and un-investigated 23-year-old primigravida who presented with chief complaints of vomiting and loose stools. The patient also complained of absent foetal movements in the last 12 hours. Investigations revealed hypokalaemia and hypomagnesemia and ultrasound revealed intra-uterine foetal demise. The patient was symptomatically relieved after electrolyte correction. Scarce reports on Gitelman’s syndrome in pregnancy have been documented with the majority of cases showing positive outcomes for the foetus. We hereby present a report of a primigravida with Gitelman’s syndrome and foetal loss which is considered uncommon.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
An improved terminology and classification of Bartter-like syndromes.
- Record: found
- Abstract: not found
- Article: not found