- Record: found
- Abstract: found
- Article: found
Prospective randomized trial of iliohypogastric-ilioinguinal nerve block on post-operative morphine use after inpatient surgery of the female reproductive tract
Read this article at
Abstract
Objective
To determine the impact of pre-operative and intra-operative ilioinguinal and iliohypogastric nerve block on post-operative analgesic utilization and length of stay (LOS).
Methods
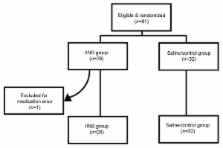
We conducted a prospective randomized double-blind placebo controlled trial to assess effectiveness of ilioinguinal-iliohypogastric nerve block (IINB) on post-operative morphine consumption in female study patients ( n = 60). Patients undergoing laparotomy via Pfannenstiel incision received injection of either 0.5% bupivacaine + 5 mcg/ml epinephrine for IINB (Group I, n = 28) or saline of equivalent volume given to the same site (Group II, n = 32). All injections were placed before the skin incision and after closure of rectus fascia via direct infiltration. Measured outcomes were post-operative morphine consumption (and associated side-effects), visual analogue pain scores, and hospital length of stay (LOS).
Results
No difference in morphine use was observed between the two groups (47.3 mg in Group I vs. 45.9 mg in Group II; p = 0.85). There was a trend toward lower pain scores after surgery in Group I, but this was not statistically significant. The mean time to initiate oral narcotics was also similar, 23.3 h in Group I and 22.8 h in Group II ( p = 0.7). LOS was somewhat shorter in Group I compared to Group II, but this difference was not statistically significant ( p = 0.8). Side-effects occurred with similar frequency in both study groups.
Conclusion
In this population of patients undergoing inpatient surgery of the female reproductive tract, utilization of post-operative narcotics was not significantly influenced by IINB. Pain scores and LOS were also apparently unaffected by IINB, indicating a need for additional properly controlled prospective studies to identify alternative methods to optimize post-surgical pain management and reduce LOS.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
The changing role of non-opioid analgesic techniques in the management of postoperative pain.
- Record: found
- Abstract: found
- Article: not found
Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials.
- Record: found
- Abstract: not found
- Article: not found