- Record: found
- Abstract: found
- Article: found
Noninvasive Imaging Tools in the Diagnosis and Treatment of Skin Cancers
Read this article at
Abstract
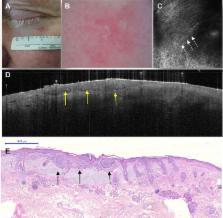
In the 1980s, the increasing incidence of skin cancers prompted the development of noninvasive medical devices to improve skin cancer diagnosis in daily dermatology practice. As a result of the development of these noninvasive techniques, diagnosis is now established earlier and with better accuracy. These advances are of great benefit to high-risk patients, who previously would have had to undergo several excisions. In this review, we focus on the classic technique of dermoscopy and the more recent digital version, as well as on advanced noninvasive imaging techniques, such as reflectance confocal microscopy and optical coherence tomography. On the basis of their specific features, these noninvasive medical devices can be used not only to diagnose and monitor melanoma and nonmelanoma skin cancers but also to choose the best therapy and follow the patient’s response to treatment in vivo.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet.
- Record: found
- Abstract: found
- Article: not found
Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi.
- Record: found
- Abstract: found
- Article: not found